Table of Contents
Results Of A Population-Based Case-Control & Case-Crossover Study
J. David Cassidy, DC, PhD, DrMedSc,*†‡ Eleanor Boyle, PhD,* Pierre Coˆte ́, DC, PhD,*†‡§ Yaohua He, MD, PhD,* Sheilah Hogg-Johnson, PhD,†§ Frank L. Silver, MD, FRCPC, and Susan J. Bondy, PhD†
SPINE Volume 33, Number 4S, pp S176 –S183 ©2008, Lippincott Williams & Wilkins
Neck pain is a common problem associated with considerable comorbidity, disability, and cost to society.1–5 In North America, the clinical management of back pain is provided mainly by medical physicians, physical therapists and chiropractors.6 Approximately 12% of American and Canadian adults seek chiropractic care annually and 80% of these visits result in spinal manipulation.7,8 When compared to those seeking medical care for back pain, Canadian chiropractic patients tend to be younger and have higher socioeconomic status and fewer health problems.6,8 In Ontario, the average number of chiropractic visits per episode of care was 10 (median 6) in 1985 through 1991.7 Several systematic reviews and our best- evidence synthesis suggest that manual therapy can benefit neck pain, but the trials are too small to evaluate the risk of rare complications.9 –13
Two deaths in Canada from vertebral artery dissection and stroke following chiropractic care in the 1990s attracted much media attention and a call by some neurologists to avoid neck manipulation for acute neck pain.14 There have been many published case reports linking neck manipulation to vertebral artery dissection15 and stroke. The prevailing theory is that extension and/or rotation of the neck can damage the vertebral artery, particularly within the foramen transversarium at the C1–C2 level. Activities leading to sudden or sustained rotation and extension of the neck have been implicated, included motor vehicle collision, shoulder checking while driving, sports, lifting, working over- head, falls, sneezing, and coughing.16 However, most cases of extracranial vertebral arterial dissection are thought to occur spontaneously, and other factors such as connective tissue disorders, migraine, hyper- tension, infection, levels of plasma homocysteine, vessel abnormalities, atherosclerosis, central venous catherization, cervical spine surgery, cervical percutaneous nerve blocks, radiation therapy and diagnostic cerebral angiography have been identified as possible risk factors.17–21
The true incidence of vertebrobasilar dissection is un- known, since many cases are probably asymptomatic, or the dissection produces mild symptoms.22 Confirming the diagnosis requires a high index of suspicion and good vascular imaging. The cases that are most likely to be diagnosed are those that result in stroke.19,22 Ischemic stroke occurs when a thrombus develops intraluminally and embolizes to more distal arteries, or less commonly, when the dissection extends distally into the intracranial vertebral artery, obliterating branching vessels.22 The best incidence estimate comes from Olmstead county, where vertebral artery dissection causing stroke affected 0.97 residents per 100,000 population between 1987 and 2003.23
To date there have been two case-control studies of stroke following neck manipulation. Rothwell et al used Ontario health data to compare 582 cases of VBA stroke to 2328 age and sex-matched controls.24 For those aged 45 years, cases were five times more likely than controls to have visited a chiropractor within 1 week of VBA stroke. Smith et al studied 51 patients with cervical artery dissection and ischemic stroke or transient ischemic attack (TIA) and compared them to 100 control patients suffering from other strokes not caused by dissections.25 Cases and controls came from two academic stroke centers in the United States and were matched on age and sex. They found no significant association between neck manipulation and ischemic stroke or TIA. However, a subgroup analysis showed that the 25 cases with vertebral artery dissection were six times more likely to have consulted a chiropractor within 30 days before their stroke than the controls.
Finally, because patients with vertebrobasilar artery dissection commonly present with headache and neck pain,23 it is possible that patients seek chiropractic care for these symptoms and that the subsequent VBA stroke occurs spontaneously, implying that the association between chiropractic care and VBA stroke is not causal.23,26 Since patients also seek medical care for headache and neck pain, any association between primary care physician (PCP) visits and VBA stroke could be attributed to seeking care for the symptoms of vertebral artery dissection.
The purpose of this study is to investigate the association between chiropractic care and VBA stroke and compare it to the association between recent PCP care and VBA stroke using two epidemiological designs. Evidence that chiropractic care increases the risk of VBA stroke would be present if the measured association between chiropractic visits and VBA stroke exceeds the association between PCP visits and VBA strokes.
Study Design
We undertook population-based case-control and case- crossover studies. Both designs use the same cases. In the case- control design, we sampled independent control subjects from the same source population as the cases. In the case-crossover design, cases served as their own controls, by sampling control periods before the study exposures.27 This design is most appropriate when a brief exposure (e.g., chiropractic care) causes a transient change in risk (i.e., hazard period) of a rare-onset disease (e.g., VBA stroke). It is well suited to our research questions, since within person comparisons control for unmeasured risk factors by design, rather than by statistical modeling.28 –30 Thus the advantage over the case control design is better control of confounding.
Source Population
The source population included all residents of Ontario (109,020,875 person-years of observation over 9 years) covered by the publicly funded Ontario Health Insurance Plan (OHIP). Available utilization data included hospitalizations with diagnostic coding, and practitioner (physician and chiropractic) utilization as documented by fee-for-service billings accompanied by diagnostic coding. We used two data sources: (1) the Discharge Abstract Database (DAD) from the Canadian Institute for Health Information, which captures hospital separations and ICD codes, and (2) the OHIP Databases for services provided by physicians and chiropractors. These data- bases can be linked from April 1992 onward.
Cases
We included all incident vertebrobasilar occlusion and stenosis strokes (ICD-9433.0 and 433.2) resulting in an acute care hospital admission from April 1, 1993 to March 31, 2002. Codes were chosen in consultation with stroke experts and an epidemiologist who participated in a similar past study (SB).24 Cases that had an acute care hospital admission for any type of stroke (ICD-9433.0, 433.2, 434, 436, 433.1, 433.3, 433.8, 433.9, 430, 431, 432, and 437.1), transient cerebral ischemia (ICD- 9435) or late effects of cerebrovascular diseases (ICD-9438) before their VBA stroke admission or since April 1, 1991 were excluded. Cases residing in long-term care facilities were also excluded. The index date was defined as the hospital admission date for the VBA stroke.
Controls
For the case-control study, four age and sex-matched controls were randomly selected from the Registered Persons Database, which contains a listing of all health card numbers for Ontario. Controls were excluded if they previously had a stroke or were residing in a long-term care facility.
For the case crossover study, four control periods were randomly chosen from the year before the VBA stroke date, using a time-stratified approach.31 The year was divided into disjoint strata with 2 week periods between the strata. For the 1 month hazard period, the disjoint strata were separated by 1 month periods and the five remaining control periods were used in the analyses. We randomly sampled disjoint strata because chiropractic care is often delivered in episodes, and this strategy eliminates overlap bias and bias associated with time trends in the exposure.32
Exposures
All reimbursed ambulatory encounters with chiropractors and PCPs were extracted for the one-year period before the index date from the OHIP database. Neck-related chiropractic visits were identified using diagnostic codes: C01–C06, cervical and cervicothoracic subluxation; C13–C15, multiple site subluxation; C30, cervical sprain/strain; C40, cervical neuritis/ neuralgia; C44, arm neuritis/neuralgia; C50, brachial radiculitis; C51, cervical radiculitis; and C60, headache. For PCP visits, we included community medicine physicians if they submitted ambulatory fee codes to OHIP. Fee codes for group therapy and signing forms were excluded. Headache or neck pain- related PCP visits were identified using the diagnostic codes: ICD-9307, tension headaches; 346, migraine headaches; 722, intervertebral disc disorders; 780, headache, except tension headache and migraine; 729, fibrositis, myositis and muscular rheumatism; and 847, whiplash, sprain/strain and other traumas associated with neck (These codes include other diagnoses, and we list only those relevant to neck pain or headache). There is no limit on the number of reimbursed PCP visits per year. However, there are limits chiropractors, but less than 15% of patients surpass them.24
Statistical Analysis
Conditional logistic regression was used to estimate the association between VBA stroke after chiropractor and PCP visits. Separate models were built using different a priori specified hazard periods, stratified by age ( 45 years and 45 years) and by visits with or without head and neck pain related diagnostic codes. For the chiropractic analysis, the index date was included in the hazard period, since chiropractic treatment might cause immediate stroke and patients would not normally consult a chiropractor after having a stroke. However, the index day was excluded from the PCP analysis, since patients might consult these physicians after experiencing a stroke. We tested different hazard periods, including 1 day, 3 days, 1 week, 2 weeks, and 1 month before the index date. Exposure occurred if any chiropractic or PCP visits were recorded during the designated hazard periods.
We also measured the effect of cumulative numbers of chiropractic and PCP visits in the month before the index date by computing the odds ratio for each incremental visit. These estimates were similarly stratified by age and by diagnostic codes related to headache and/or neck pain. Finally, we conducted analyses to determine if our results were sensitive to chiropractic and PCP visits related to neck complaints and headaches. We report our results as odds ratios (OR) and 95% confidence intervals. Confidence intervals were estimated by accelerated bias corrected bootstraps with 2000 replications using the variance co-variance method.33 All statistical analyses were per- formed using STATA/SE version 9.2.34
Results
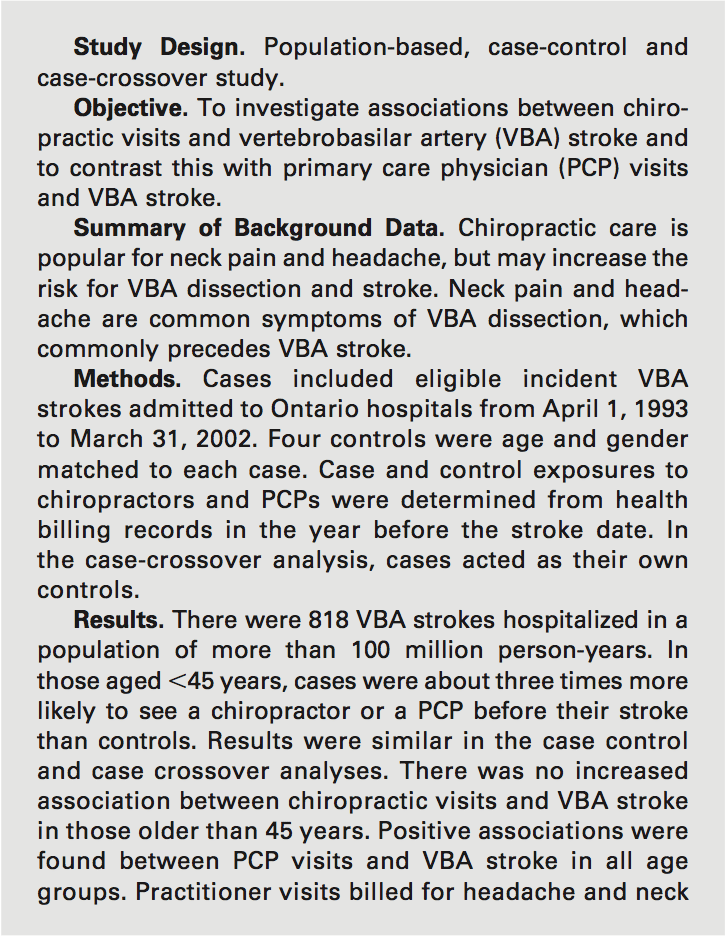
A total of 818 VBA strokes met our inclusion/exclusion criteria over the 9 year inception period. Of the 3272 matched control subjects, 31 were excluded because of prior stroke, one had died before the index date and 76 were receiving long-term care. Thus, 3164 control subjects were matched to the cases. The mean age of cases and controls was 63 years at the index date and 63% were male. Cases had a higher proportion of comorbid conditions (Table 1). Of the 818 stroke cases, 337 (41.2%) were coded as basilar occlusion and stenosis, 443 (54.2%) as vertebral occlusion and stenosis and 38 (4.7%) had both codes.
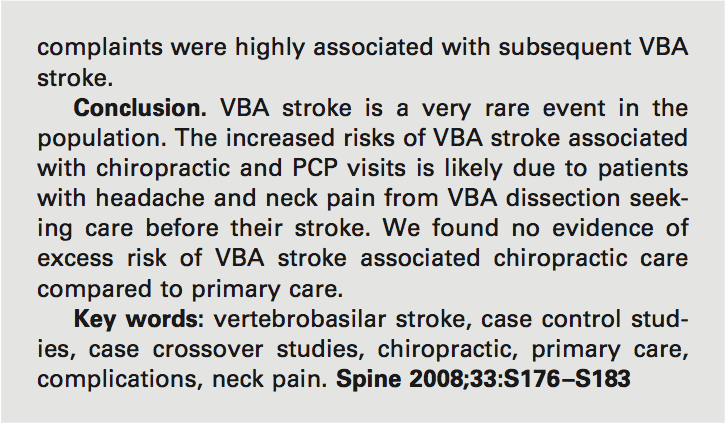
 Overall, 4% of cases and controls had visited a chiropractor within 30 days of the index date, while 53% of cases and 30% of controls had visited a PCP within that time (Table 2). For those under 45 years of age, 8 cases (7.8%) had consulted a chiropractor within 7 days of the index date, compared to 14 (3.4%) of controls. For PCPs, 25 cases (24.5%) under 45 years of age had a consultation within 7 days of the index date, com- pared to 27 (6.6%) of controls. With respect to the number of visits within 1 month of the index date, 7.8% of cases under the age of 45 years had three or more chiropractic visits, whereas 5.9% had three or more PCP visits (Table 2).
Overall, 4% of cases and controls had visited a chiropractor within 30 days of the index date, while 53% of cases and 30% of controls had visited a PCP within that time (Table 2). For those under 45 years of age, 8 cases (7.8%) had consulted a chiropractor within 7 days of the index date, compared to 14 (3.4%) of controls. For PCPs, 25 cases (24.5%) under 45 years of age had a consultation within 7 days of the index date, com- pared to 27 (6.6%) of controls. With respect to the number of visits within 1 month of the index date, 7.8% of cases under the age of 45 years had three or more chiropractic visits, whereas 5.9% had three or more PCP visits (Table 2).
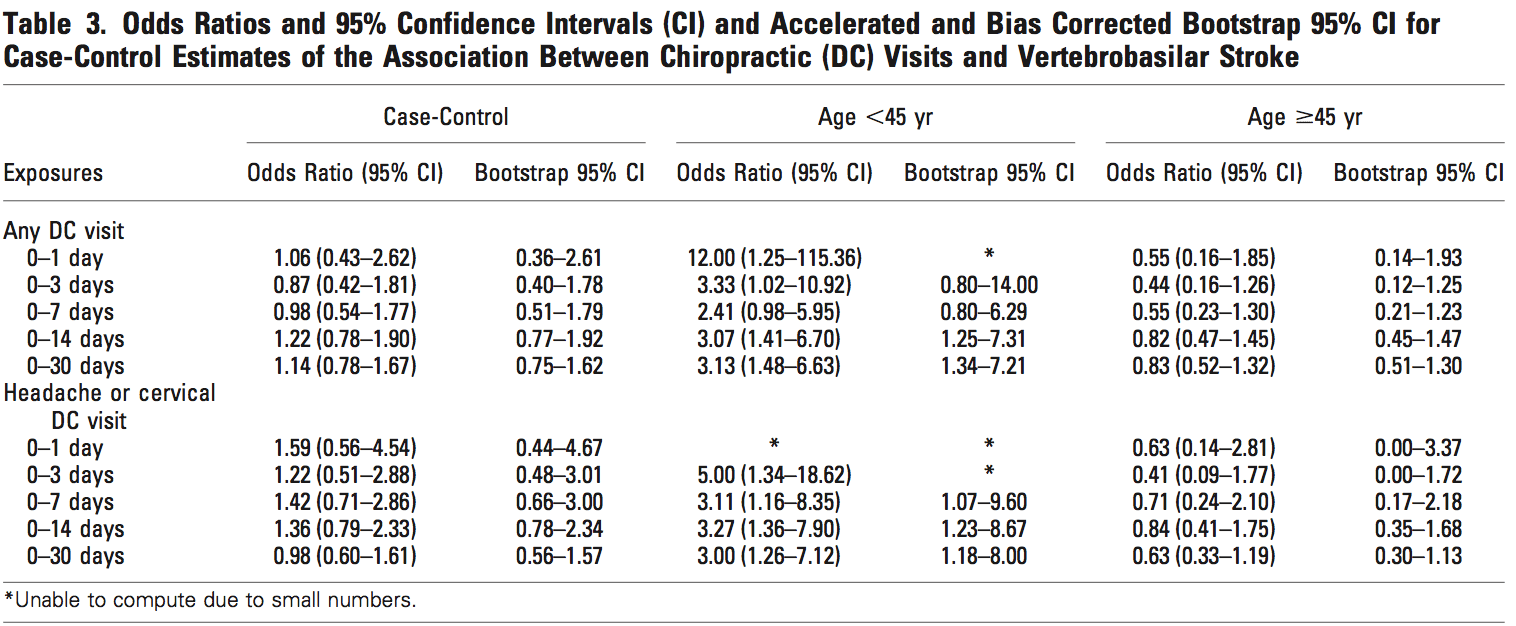
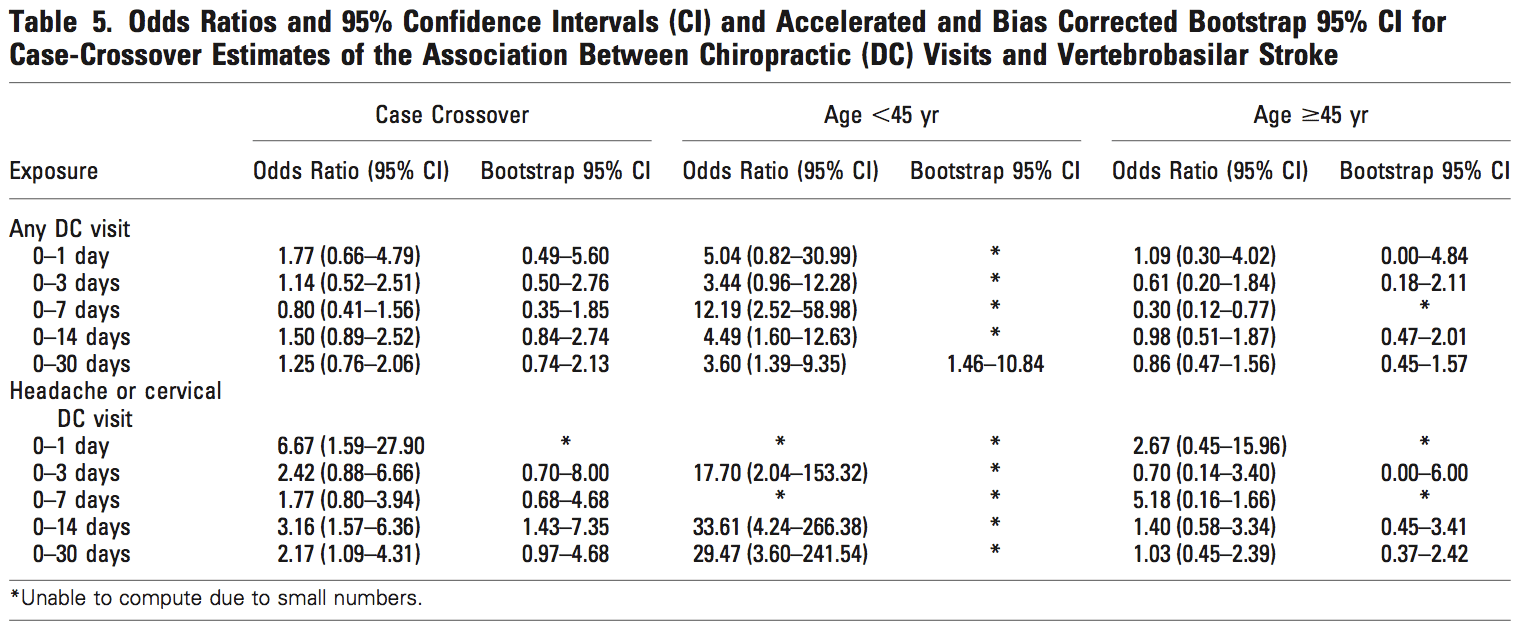
 The case control and case crossover analyses gave similar results. (Tables 3–7) Age modified the effect of chiropractic visits on the risk of VBA stroke. For those under 45 years of age, there was an increased association between chiropractic visits and VBA stroke regardless of the hazard period. For those 45 years of age and older, there was no association. Each chiropractic visit in the month before the index date was associated with an in- creased risk of VBA stroke in those under 45 years of age (OR 1.37; 95% CI 1.04–1.91 from the case crossover analysis) (Table 7). We were not able to estimate boot- strap confidence intervals in some cases because of sparse data.
The case control and case crossover analyses gave similar results. (Tables 3–7) Age modified the effect of chiropractic visits on the risk of VBA stroke. For those under 45 years of age, there was an increased association between chiropractic visits and VBA stroke regardless of the hazard period. For those 45 years of age and older, there was no association. Each chiropractic visit in the month before the index date was associated with an in- creased risk of VBA stroke in those under 45 years of age (OR 1.37; 95% CI 1.04–1.91 from the case crossover analysis) (Table 7). We were not able to estimate boot- strap confidence intervals in some cases because of sparse data.
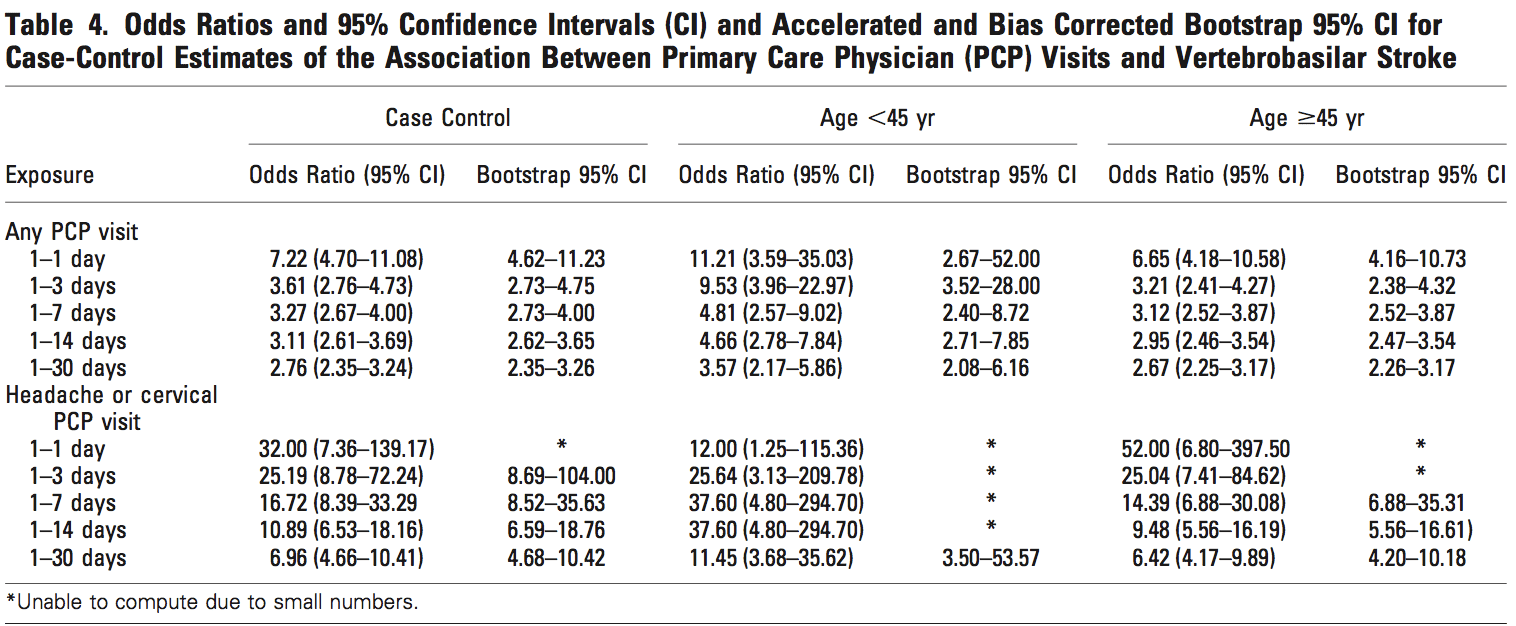
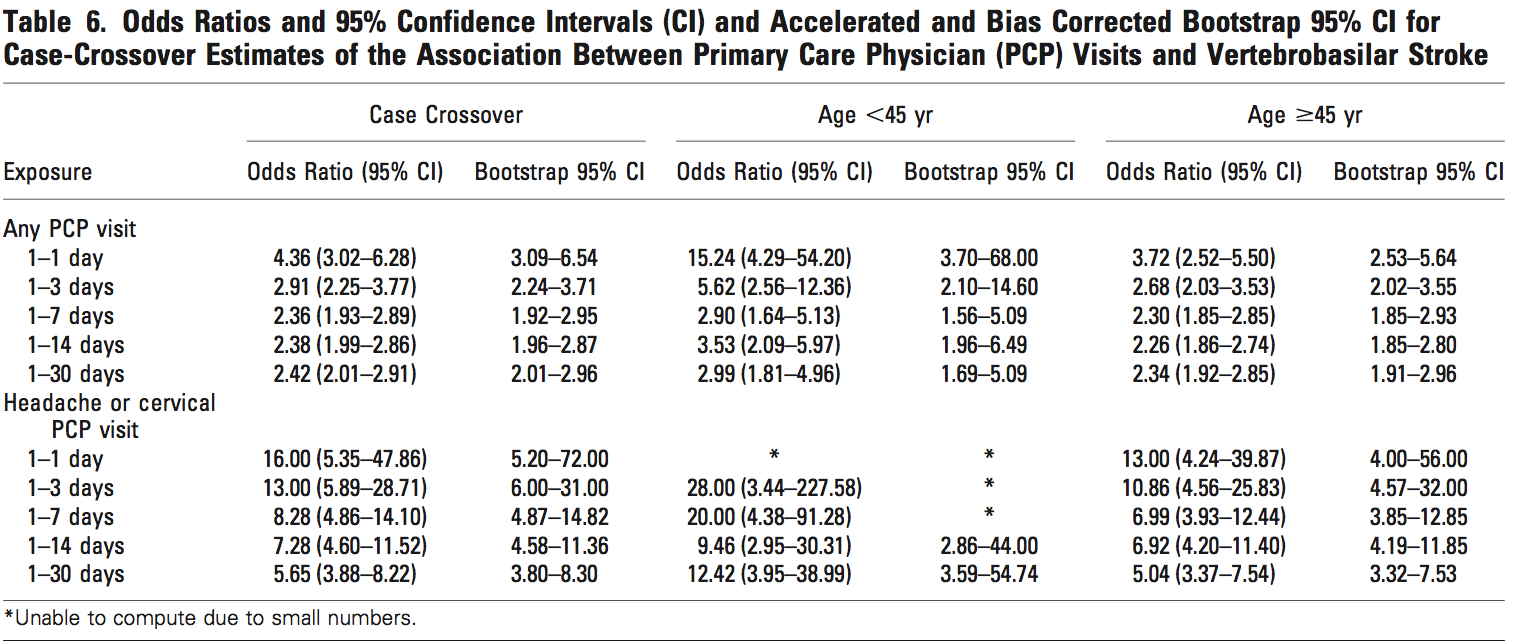
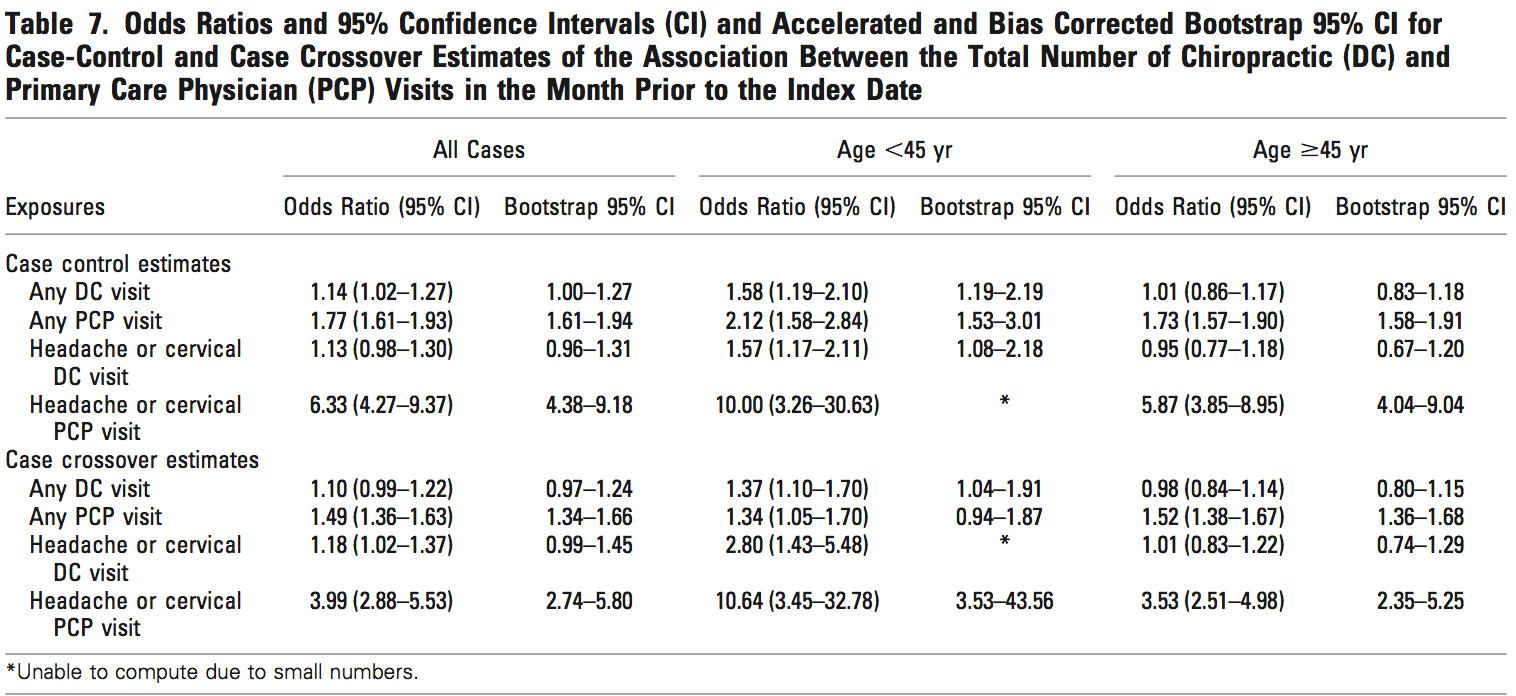 Similarly, we found that visiting a PCP in the month before the index date was associated with an increased risk of VBA stroke regardless of the hazard period, or the age of the subject. Each PCP visit in the month before the stroke was associated with an increased risk of VBA stroke both in those under 45 years of age (OR 1.34; 95% CI 0.94 –1.87 from the case crossover analysis) and 45 years and older (OR 1.52; 95% CI 1.36–1.67 from the case crossover analysis) (Table 7).
Similarly, we found that visiting a PCP in the month before the index date was associated with an increased risk of VBA stroke regardless of the hazard period, or the age of the subject. Each PCP visit in the month before the stroke was associated with an increased risk of VBA stroke both in those under 45 years of age (OR 1.34; 95% CI 0.94 –1.87 from the case crossover analysis) and 45 years and older (OR 1.52; 95% CI 1.36–1.67 from the case crossover analysis) (Table 7).
Our results were sensitive to chiropractic and PCP visits related to neck complaints and headaches, and we observed sharp increases in the associations when restricting the analyses to these visits (Tables 3–7). Overall, these associations were more pronounced in the PCP analyses. However, the data are sparse, and we were unable to compute bootstrap confidence intervals in many cases.
Discussion
Our study advances knowledge about the association between chiropractic care and VBA stroke in two respects. First, our case control results agree with past case control studies that found an association between chiropractic care and vertebral artery dissection and VBA stroke.24,25 Second, our case crossover results confirm these findings using a stronger research design with better control of confounding variables. The case-crossover design controls for time independent confounding factors, both known and unknown, which could affect the risk of VBA stroke. This is important since smoking, obesity, undiagnosed hypertension, some connective tis- sue disorders and other important risk factors for dissection and VBA stroke are unlikely to be recorded in ad- ministrative databases.
We also found strong associations between PCP visits and subsequent VBA stroke. A plausible explanation for this is that patients with head and neck pain due to vertebral artery dissection seek care for these symptoms, which precede more than 80% of VBA strokes.23 Since it is unlikely that PCPs cause stroke while caring for these patients, we can assume that the observed association between recent PCP care and VBA stroke represents the background risk associated with patients seeking care for dissection-related symptoms leading to VBA stroke. Be- cause the association between chiropractic visits and VBA stroke is not greater than the association between PCP visits and VBA stroke, there is no excess risk of VBA stroke from chiropractic care.
Our study has several strengths and limitations. The study base includes an entire population over a 9-year period representing 109,020,875 person-years of observation. Despite this, we found only 818 VBA strokes, which limited our ability to compute some estimates and bootstrap confidence intervals. In particular, our age stratified analyses are based on small numbers of ex- posed cases and controls (Table 2). Further stratification by diagnostic codes for headache and neck pain related visits imposed even greater difficulty with these estimates. However, there are few databases that can link incident VBA strokes with chiropractic and PCP visits in a large enough population to undertake a study of such a rare event.
A major limitation of using health administrative data are misclassification bias, and the possibility of bias in assignment of VBA-related diagnoses, which has previously been raised in this context.24 Liu et al have shown that ICD-9 hospital discharge codes for stroke have a poor positive predictive value when compared to chart review.35 Furthermore, not all VBA strokes are secondary to vertebral artery dissection and administrative databases do not provide the clinical detail to determine the specific cause. To investigate this bias, we did a sensitivity analysis using different positive predictive values for stroke diagnosis (ranging from 0.2 to 0.8). Assuming non differential misclassification of chiropractic and PCP cases, our analysis showed attenuation of the estimates towards the null with lower positive predictive values, but the conclusions did not change (i.e., associations remained positive and significant—data not shown). The reliability and validity of the codes to classify headache and cervical visits to chiropractors and PCPs is not known.
It is also possible that patients presenting to hospital with neurologic symptoms who have recently seen a chiropractor might be subjected to a more vigorous diagnostic workup focused on VBA stroke (i.e., differential misclassification).36 In this case, the predictive values of the stroke codes would be greater for cases that had seen a chiropractor and our results would underestimate the association between PCP care and VBA stroke.
A major strength of our study is that exposures were measured independently of case definition and handled identically across cases and controls. However, there was some overlap between chiropractic care and PCP care. In the month before their stroke, only 16 (2.0%) of our cases had seen only a chiropractor, while 20 (2.4%) had seen both a chiropractor and PCP, and 417 (51.0%) had just seen only a PCP. We were not able to run a subgroup analysis on the small number of cases that just saw a chiropractor. However, subgroup analysis on the PCP cases (n 782) that did not visit a chiropractors during the 1 month before their stroke did not change the conclusions (data not shown).
Our results should be interpreted cautiously and placed into clinical perspective. We have not ruled out neck manipulation as a potential cause of some VBA strokes. On the other hand, it is unlikely to be a major cause of these rare events. Our results suggest that the association between chiropractic care and VBA stroke found in previous studies is likely explained by present- ing symptoms attributable to vertebral artery dissection. It might also be possible that chiropractic manipulation, or even simple range of motion examination by any practitioner, could result in a thromboembolic event in a patient with a pre-existing vertebral dissection. Unfortunately, there is no acceptable screening procedure to identify patients with neck pain at risk of VBA stroke.37 These events are so rare and difficult to diagnose that future studies would need to be multi-centered and have unbiased ascertainment of all potential exposures. Given our current state of knowledge, the decision of how to treat patients with neck pain and/or headache should be driven by effectiveness and patient preference.38
Conclusion
Our population-based case-control and case-crossover study shows an association between chiropractic visits and VBA strokes. However, we found a similar association between primary care physician visits and VBA stroke. This suggests that patients with undiagnosed vertebral artery dissection are seeking clinical care for head- ache and neck pain before having a VBA stroke.
Acknowledgments
The authors acknowledge the members of the Decade of the Bone and Joint 2000 –2010 Task Force on Neck Pain and its Associate Disorders for advice about de- signing this study. In particular, they acknowledge the help of Drs. Hal Morgenstern, Eric Hurwitz, Scott Haldeman, Linda Carroll, Gabrielle van der Velde, Lena Holm, Paul Peloso, Margareta Nordin, Jaime Guzman, Eugene Carragee, Rachid Salmi, Alexander Grier, and Mr. Jon Schubert.
References
1. Borghouts JA, Koes BW, Vondeling H, et al. Cost-of-illness of neck pain in The Netherlands in 1996. Pain 1999;80:629–36.
2. Coˆte´ P, Cassidy JD, Carroll L. The Saskatchewan Health and Back PainSurvey. The prevalence of neck pain and related disability in Saskatchewan adults. Spine 1998;23:1689–98.
3. Coˆte´ P, Cassidy JD, Carroll L. The factors associated with neck pain and its related disability in the Saskatchewan population. Spine 2000;25:1109–17.
4. Coˆte´ P, Cassidy JD, Carroll L. Is a lifetime history of neck injury in a trafficcollision associated with prevalent neck pain, headache and depressive symptomatology? Accid Anal Prev 2000;32:151–9.
5. Coˆte´ P, Cassidy JD, Carroll LJ, et al. The annual incidence and course of neck pain in the general population: a population-based cohort study. Pain 2004; 112:267–73.
6. Coˆte´ P, Cassidy JD, Carroll L. The treatment of neck and low back pain: who seeks care? who goes where? Med Care 2001;39:956–67.
7. Hurwitz EL, Coulter ID, Adams AH, et al. Use of chiropractic services from 1985 through 1991 in the United States and Canada. Am J Public Health1998;88:771–6.
8. Hurwitz EL, Chiang LM. A comparative analysis of chiropractic and general practitioner patients in North America: findings from the jointCanada/United States Survey of Health, 2002–03. BMC Health Serv Res 2006;6:49.
9. Aker PD, Gross AR, Goldsmith CH, et al. Conservative management of mechanical neck pain: systematic overview and meta-analysis. BMJ 1996; 313:1291–6.
10. Gross AR, Kay T, Hondras M, et al. Manual therapy for mechanical neckdisorders: a systematic review. Man Ther 2002;7:131–49.
11. Hurwitz EL, Aker PD, Adams AH, et al. Manipulation and mobilization of the cervical spine. A systematic review of the literature. Spine 1996;21:1746–59.
12. McClune T, Burton AK, Waddell G. Whiplash associated disorders: a review of the literature to guide patient information and advice. Emerg Med J 2002;19:499–506.
13. Peeters GG, Verhagen AP, de Bie RA, et al. The efficacy of conservative treatment in patients with whiplash injury: a systematic review of clinical trials. Spine 2001;26:E64–E73.
14. Norris JW, Beletsky V, Nadareishvili ZG. Sudden neck movement and cervical artery dissection. The Canadian Stroke Consortium. CMAJ 2000;163:38–40.
15. Ernst E. Manipulation of the cervical spine: a systematic review of case reports of serious adverse events, 1995–2001. Med J Aust 2002;176:376–80.
16. Haldeman S, Kohlbeck FJ, McGregor M. Risk factors and precipitating neckmovements causing vertebrobasilar artery dissection after cervical trauma and spinal manipulation. Spine 1999;24:785–94.
17. Rubinstein SM, Peerdeman SM, van Tulder MW, et al. A systematic reviewof the risk factors for cervical artery dissection. Stroke 2005;36:1575–80.
18. Inamasu J, Guiot BH. Iatrogenic vertebral artery injury. Acta Neurol Scand 2005;112:349–57.
19. Schievink WI. Spontaneous dissection of the carotid and vertebral arteries. N Engl J Med 2001;344:898–906.
20. D’Anglejan-Chatillon J, Ribeiro V, Mas JL, et al. Migraine—a risk factor for dissection of cervical arteries. Headache 1989;29:560–1.
21. Pezzini A, Caso V, Zanferrari C, et al. Arterial hypertension as risk factor for spontaneous cervical artery dissection. A case-control study. J Neurol Neurosurg Psychiatry 2006;77:95–7.
22. Savitz SI, Caplan LR. Vertebrobasilar disease. N Engl J Med 2005;352: 2618–26.
23. Lee VH, Brown RD Jr, Mandrekar JN, et al. Incidence and outcome of cervical artery dissection: a population-based study. Neurology 2006;67: 1809–12.
24. Rothwell DM, Bondy SJ, Williams JI. Chiropractic manipulation and stroke: a population-based case-control study. Stroke 2001;32:1054–60.
25. Smith WS, Johnston SC, Skalabrin EJ, et al. Spinal manipulative therapy is an independent risk factor for vertebral artery dissection. Neurology 2003;60: 1424–8.
26. Arnold M, Bousser MG, Fahrni G, et al. Vertebral artery dissection: presenting findings and predictors of outcome. Stroke 2006;37:2499–503.
27. Maclure M. The case-crossover design: a method for studying transient effects on the risk of acute events. Am J Epidemiol 1991;133:144–53.
28. Kelman CW, Kortt MA, Becker NG, et al. Deep vein thrombosis and air travel: record linkage study. BMJ 2003;327:1072.
29. Mittleman MA, Maclure M, Tofler GH, et al. Triggering of acute myocardial infarction by heavy physical exertion. Protection against triggering by regular exertion. Determinants of Myocardial Infarction Onset Study Investigators.
N Engl J Med 1993;329:1677–83.
30. Redelmeier DA, Tibshirani RJ. Association between cellular-telephone calls and motor vehicle collisions. N Engl J Med 1997;336:453–8.
31. Janes H, Sheppard L, Lumley T. Overlap bias in the case-crossover design, with application to air pollution exposures. Stat Med 2005;24:285–300.
32. Janes H, Sheppard L, Lumley T. Case-crossover analyses of air pollution exposure data: referent selection strategies and their implications for bias. Epidemiology 2005;16:717–26.
33. Efron B, Tibshirani RJ. An Introduction to the Bootstrap. New York: Chapmanand Hall/CRC, 1993.
34. STATA/SE [computer program]. College Station, Tex: Stata Corp, 2006.
35. Liu L, Reeder B, Shuaib A, et al. Validity of stroke diagnosis on hospitaldischarge records in Saskatchewan, Canada: implications for stroke surveillance. Cerebrovasc Dis 1999;9:224–30.
36. Boyle E, Coˆte´ P, Grier AR, et al. Examining vertebrobasilar artery stroke in two Canadian provinces. Spine, in press.
37. Coˆte´ P, Kreitz BG, Cassidy JD, et al. The validity of the extension-rotation test as a clinical screening procedure before neck manipulation: a secondary analysis. J Manip Physiol Therap 1996;159–64.
38. van der Velde G, Hogg-Johnson S, Bayoumi A, et al. Identifying the best treatment among common non-surgical neck pain treatments: a decision analysis. Spine 2008;33(Suppl):S184–S191.
Key words: vertebrobasilar stroke, case control stud- ies, case crossover studies, chiropractic, primary care, complications, neck pain. Spine 2008;33:S176–S183
From the *Centre of Research Expertise for Improved Disability Outcomes (CREIDO), University Health Network Rehabilitation Solutions, Toronto Western Hospital, and the Division of Heath Care and Outcomes Research, Toronto Western Research Institute, Toronto, ON, Canada; †Department of Public Health Sciences, Management and Evaluation, University of Toronto, Toronto, ON, Canada; ‡Department of Health Policy, Management and Evalua- tion, University of Toronto, Toronto, ON, Canada; §Institute for Work & Health, Toronto, ON, Canada; ¶University Health Net- work Stroke Program, Toronto Western Hospital, Toronto, ON, Canada; and Division of Neurology, Department of Medicine, Fac- ulty of Medicine, University of Toronto, Toronto, ON, Canada. Supported by Ontario Ministry of Health and Long-term Care. P.C. is supported by the Canadian Institute of Health Research through a New Investigator Award. S.H.-J. is supported by the Institute for Work & Health and the Workplace Safety and Insurance Board of Ontario. The opinions, results, and conclusions are those of the authors and no endorsement by the Ministry is intended or should be inferred.
The manuscript submitted does not contain information about medical device(s)/drug(s).
University Health Network Research Ethics Board Approval number 05-0533-AE.
Address correspondence and reprint requests to J. David Cassidy, DC, PhD, DrMedSc, Toronto Western Hospital, Fell 4-114, 399 Bathurst Street, Toronto, ON, Canada M5T 2S8; E-mail: [email protected]
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card



Comments are closed.