Table of Contents
Introduction
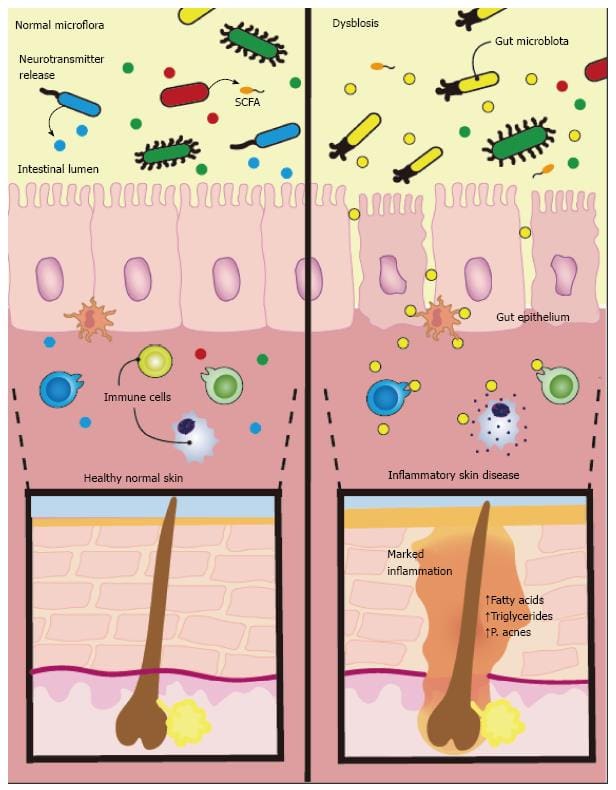
The skin is the largest organ in the body and encounters numerous factors that can either benefit or harm the body. The skin helps protect the organs and intestines in the gut system, keeps the musculoskeletal system structure functional, and even helps the nervous system send out signals for motor-sensory functions to the rest of the body. The skin is associated with the gut system as the gut microbiota host trillions of beneficial gut flora that send out nutrients to help promote tissue growth, improve the body’s immunity, and metabolize skin health by protecting it from disruptive pathogens. When these pathogens cause inflammatory issues in the gut system, it can affect the body’s skin, brain, and immune health by making them dysfunctional. Today’s article will look at a skin condition known as atopic dermatitis, how it affects the gut-skin system, and what treatments are available for relieving gut issues and atopic dermatitis in individuals. Referring patients to certified, skilled providers who specialize in gastroenterology treatments. We provide guidance to our patients by referring to our associated medical providers based on their examination when it’s appropriate. We find that education is critical for asking insightful questions to our providers. Dr. Alex Jimenez DC provides this information as an educational service only. Disclaimer
Can my insurance cover it? Yes, it may. If you are uncertain, here is the link to all the insurance providers we cover. If you have any questions or concerns, please call Dr. Jimenez at 915-850-0900.
What Is Atopic Dermatitis?
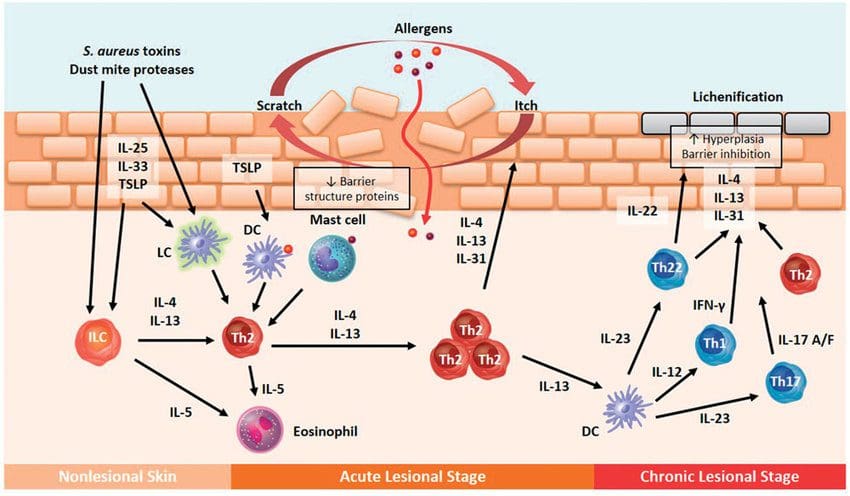
Have you experienced inflammation around your gut or in certain areas of your skin? Do issues like SIBO, IBD, leaky gut, or bloating become more frequent? Do certain foods trigger inflammatory markers in your skin and gut? The numerous signs and symptoms are due to a skin disorder known as atopic dermatitis. Atopic dermatitis or eczema is a pruritic, hereditary skin disorder. The lifetime prevalence is 10% to 20%, with many cases starting as a baby and rising to 20% to 40% as adults continue to have atopic dermatitis. Research studies have defined atopic dermatitis as one of the most common skin diseases that cause chronic inflammation in the skin. The pathophysiology of atopic dermatitis is both complex and multifactorial. It involves the elements of barrier dysfunction, alterations in cell-mediated immune responses, IgE-mediated hypersensitivity, and environmental factors that cause flare-ups. Additional research studies have mentioned that the pathology of atopic dermatitis is being looked at as the skin’s structural abnormalities and immune dysregulation play their roles as this condition progress. Other genetic changes have also been identified, altering the skin’s barrier function, resulting in an atopic dermatitis phenotype. The imbalance of Th2 to Th1 cytokines is observed as it alters cell-mediated immune responses. Atopic dermatitis can promote IgE-mediated hypersensitivity in the skin as part of its development. This can also be due to the environmental factors that be the causing development of atopic dermatitis.
How Does It Affect The Gut-Skin Connection?
Since atopic dermatitis is a chronic inflammatory skin disease, many factors do come to play in its development. For example, food allergies cause atopic dermatitis in 25% to 50% of children. Some of the food allergens that are commonly linked to atopic dermatitis include:
- Eggs
- Soy
- Milk
- Wheat
- Fish
- Shellfish
- Peanuts
One of the other factors that can cause the development of atopic dermatitis is gut issues. Research studies have shown that any alterations in the gut microbiome due to atopic dermatitis affect the immune system balance in the body. When the gut microbiome becomes altered, it affects metabolite production and reduces the body’s immune system. When bacteria overgrowth in the GI tract, it has been suggested as a causative factor in allergic diseases, including atopic dermatitis. Another factor is when individuals consume trans fats, which increase the development of atopic dermatitis since they interfere with the metabolism and use of essential fatty acids.
The Microbiome Of Atopic Dermatitis-Video
Have you experienced inflammation in your digestive tract or particular areas of your skin? Does your body feel fatigued constantly? Do you have any gut issues or disorders that are affecting your health? Most of these symptoms are signs that you are experiencing atopic dermatitis caused by gut issues. Research studies have found that various factors can trigger atopic dermatitis, affect the immune system, and disrupt the gut microbiota. The video above explains the microbiome in atopic dermatitis and how it affects the gut, skin, and the entire body. Luckily there are available treatments to relieve atopic dermatitis and gut disorders from wreaking havoc on the body.
Treatments For Relieving Atopic Dermatitis & The Gut
When a person begins to find treatments for relieving atopic dermatitis usually involves:
- Early diagnosis.
- Skin barrier function support.
- Mitigation of cutaneous inflammation.
- Concomitant risk stratification
Another way that many individuals can alleviate atopic dermatitis is with a healthy GI tract. This will help many individuals suffering from a food allergy, asthma, allergic rhinitis, and environmental allergies to relieve atopic dermatitis from progressing further. A study showed that probiotics and prebiotics are essential in preventing food allergies and eczema. Probiotics and prebiotics help replenish the beneficial bacteria in the gut and regulate the immune system. This prevents atopic dermatitis from stopping progressing and restor the body back.
Conclusion
Many factors cause atopic dermatitis progression to become severe, as it is crucial to find the root cause of the flare-ups and alleviate them at the source. Overall having gut issues associated with atopic dermatitis is no laughing matter. When the gut microbiome is being affected by inflammatory disorders, it can disrupt the immune system and cause atopic dermatitis to develop on the skin. Incorporating probiotics and prebiotics can help replenish the gut bacteria and figure out what causes the inflammatory symptoms to spike up from certain foods will benefit the gut and the skin to become healthier.
References
Fang, Zhifeng, et al. “Gut Microbiota, Probiotics, and Their Interactions in Prevention and Treatment of Atopic Dermatitis: A Review.” Frontiers in Immunology, Frontiers Media S.A., 14 July 2021, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8317022/.
Kapur, Sandeep, et al. “Atopic Dermatitis.” Allergy, Asthma, and Clinical Immunology : Official Journal of the Canadian Society of Allergy and Clinical Immunology, BioMed Central, 12 Sept. 2018, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6157251/.
Kim, Jung Eun, and Hei Sung Kim. “Microbiome of the Skin and Gut in Atopic Dermatitis (AD): Understanding the Pathophysiology and Finding Novel Management Strategies.” Journal of Clinical Medicine, MDPI, 2 Apr. 2019, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6518061/.
Kolb, Logan, and Sarah J Ferrer-Bruker. “Atopic Dermatitis – Statpearls – NCBI Bookshelf.” In: StatPearls [Internet]. Treasure Island (FL), StatPearls Publishing, 13 Aug. 2021, https://www.ncbi.nlm.nih.gov/books/NBK448071/.
Lee, So Yeon, et al. “Microbiome in the Gut-Skin Axis in Atopic Dermatitis.” Allergy, Asthma & Immunology Research, The Korean Academy of Asthma, Allergy and Clinical Immunology; The Korean Academy of Pediatric Allergy and Respiratory Disease, July 2018, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6021588/.
Disclaimer
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card



Comments are closed.