Common Injuries and Treatment for the Plantaris Muscle
Individuals who engage in sports and physical activities that involve lunging forward while running or jumping can sustain a plantaris muscle injury. Can understanding the anatomy of the back of the leg and the symptoms help diagnose and treat plantar muscle injuries?
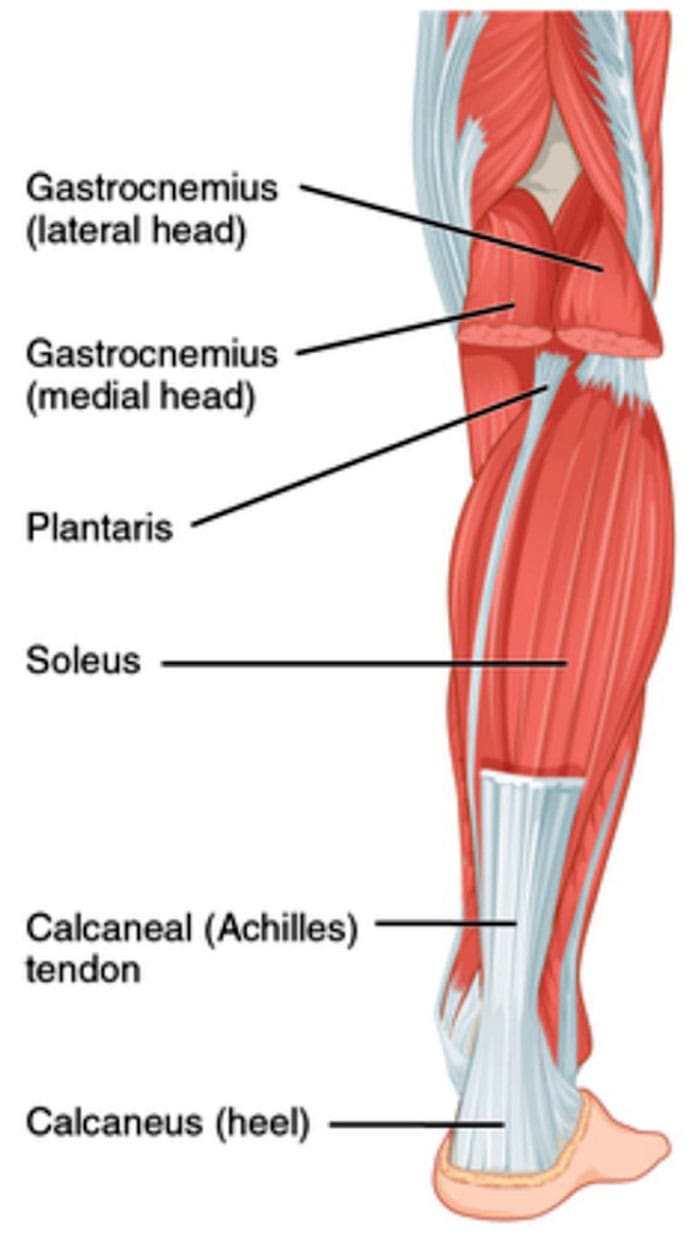
Table of Contents
Plantaris Muscle
The plantaris muscle is a long, narrow muscle in the calf that runs along the back of the leg. It’s part of the Triceps Surae, a group of muscles in the calf that, along with the gastrocnemius and soleus muscles, makes up the bulk of the back of the leg. It is located in the superficial posterior compartment of the leg. Strains or tears of the plantaris muscle at the back of the leg can cause pain and swelling, similar to a calf strain or Achilles tendon tear. Individuals may feel immediate pain, cramping, and other symptoms.
Anatomy
The gastrocnemius and soleus muscles are the major muscles, with the soleus located deeper in the leg. Together, they form the Achilles tendon, which blends into a tendon in the back of the heel and attaches to the heel bone/calcaneus. When the calf muscles contract, they point the foot downward, propelling the body forward when walking, running, and sprinting. The plantaris muscle and tendon sit more or less in the center of the calf, between the two heads of the gastrocnemius. Around 7% to 20% of the population are born without plantaris muscles. There are variations, such as having a double- or triple-headed plantaris muscle. (Olewnik Ł. et al., 2020) However, individuals that do not have the muscle or have a variation have not been shown to affect long-term or short-term mobility.
Symptoms
Plantaris muscle ruptures are the most common injury and occur often during running or jumping. (Spang C. et al., 2016) Many who sustain this injury are athletes who have to lunge forward. Common symptoms include:
- Sudden onset pain behind the calf.
- Swelling of the calf muscle.
- Muscle knots or myofascial trigger points of the calf muscle.
- Swelling and bruising in the back of the calf area.
- Cramping in the calf muscle.
- Spasm sensations of the calf muscle.
- Symptoms of a plantaris muscle strain are less severe, with the common signs being tightness and pain during and after physical activity.
Diagnosis
Plantaris muscle tears differ from Achilles tendon tears because the foot can be pointed downward following the rupture, whereas an Achilles tear cannot. Plantaris ruptures can also be confused with a blood clot in the large veins of the calf, called deep vein thrombosis/DVT. (Rohilla S. et al., 2013) Tests like MRI or ultrasound can be performed to confirm or exclude a plantaris rupture. Both can be useful for verifying whether the injury is a strain or tear and identifying other possible causes of calf pain.
Treatment
Treatment is typically non-surgical. While the injuries can cause pain and disability, the symptoms almost always resolve with conservative treatments and therapies. Rest, ice, compression, and elevation are the first line used and may be all that is needed for a muscle strain. Short-term use of NSAIDs may be recommended for a strain or tear to reduce pain and inflammation. (Morelli K. M. et al., 2018) If the pain is profound or there is a tear, patients may require short-term immobilization or the use of a crutch for the pain to subside. With the assistance of a physical therapist, sports chiropractor, and athletic trainer, gradual increases in mobility and strength can be obtained. Symptoms usually gradually resolve over several weeks. Full recovery may take up to eight weeks, depending on the severity of the injury.
Injury Medical Chiropractic and Functional Medicine Clinic works with primary healthcare providers and specialists to develop customized treatment programs through an integrated approach to treating injuries and chronic pain syndromes, improving flexibility, mobility, and agility, relieving pain, and helping individuals return to normal activities. If other treatments are needed, Dr. Jimenez has teamed up with top surgeons, clinical specialists, medical researchers, and rehabilitation providers to provide the most effective treatments.
Control Foot Motion with Custom Orthotics
References
Olewnik, Ł., Zielinska, N., Karauda, P., Tubbs, R. S., & Polguj, M. (2020). A three-headed plantaris muscle: evidence that the plantaris is not a vestigial muscle?. Surgical and radiologic anatomy : SRA, 42(10), 1189–1193. https://doi.org/10.1007/s00276-020-02478-8
Spang, C., Alfredson, H., Docking, S. I., Masci, L., & Andersson, G. (2016). The plantaris tendon: a narrative review focusing on anatomical features and clinical importance. The bone & joint journal, 98-B(10), 1312–1319. https://doi.org/10.1302/0301-620X.98B10.37939
Rohilla, S., Jain, N., & Yadav, R. (2013). Plantaris rupture: why is it important?. BMJ case reports, 2013, bcr2012007840. https://doi.org/10.1136/bcr-2012-007840
Morelli, K. M., Brown, L. B., & Warren, G. L. (2018). Effect of NSAIDs on Recovery From Acute Skeletal Muscle Injury: A Systematic Review and Meta-analysis. The American journal of sports medicine, 46(1), 224–233. https://doi.org/10.1177/0363546517697957
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card



Comments are closed.