[et_pb_section bb_built=”1″][et_pb_row][et_pb_column type=”4_4″][et_pb_text]
Headache pain is one of the most prevalent reasons for doctor office visits. The majority of people experience them at some point in their life and they can affect anyone, regardless of age, race and gender. The International Headache Society, or IHS, categorizes headaches as primary, when they are not caused by another injury and/or condition, or secondary, when there is an underlying cause behind them. From migraines to cluster headaches and tension headaches, people who suffer from constant head pain may find it difficult to participate in their everyday activities. Many healthcare professionals treat headache pain, however, chiropractic care has become a popular alternative treatment option for a variety of health issues. The purpose of the following article is to demonstrate evidence-based guidelines for the chiropractic treatment of adults with headache.
Table of Contents
Evidence-Based Guidelines for the Chiropractic Treatment of Adults with Headache
Abstract
- Objective: The purpose of this manuscript is to provide evidence-informed practice recommendations for the chiropractic treatment of headache in adults.
- Methods: Systematic literature searches of controlled clinical trials published through August 2009 relevant to chiropractic practice were conducted using the databases MEDLINE; EMBASE; Allied and Complementary Medicine; the Cumulative Index to Nursing and Allied Health Literature; Manual, Alternative, and Natural Therapy Index System; Alt HealthWatch; Index to Chiropractic Literature; and the Cochrane Library. The number, quality, and consistency of findings were considered to assign an overall strength of evidence (strong, moderate, limited, or conflicting) and to formulate practice recommendations.
- Results: Twenty-one articles met inclusion criteria and were used to develop recommendations. Evidence did not exceed a moderate level. For migraine, spinal manipulation and multimodal multidisciplinary interventions including massage are recommended for management of patients with episodic or chronic migraine. For tension-type headache, spinal manipulation cannot be recommended for the management of episodic tension-type headache. A recommendation cannot be made for or against the use of spinal manipulation for patients with chronic tension-type headache. Low-load craniocervical mobilization may be beneficial for longer term management of patients with episodic or chronic tension-type headaches. For cervicogenic headache, spinal manipulation is recommended. Joint mobilization or deep neck flexor exercises may improve symptoms. There is no consistently additive benefit of combining joint mobilization and deep neck flexor exercises for patients with cervicogenic headache. Adverse events were not addressed in most clinical trials; and if they were, there were none or they were minor.
- Conclusions: Evidence suggests that chiropractic care, including spinal manipulation, improves migraine
and cervicogenic headaches. The type, frequency, dosage, and duration of treatment(s) should be based on guideline recommendations, clinical experience, and findings. Evidence for the use of spinal manipulation as an isolated intervention for patients with tension-type headache remains equivocal. (J Manipulative Physiol Ther 2011;34:274-289) - Key Indexing Terms: Spinal Manipulation; Migraine Disorders; Tension-Type Headache; Post-traumatic Headache; Practice Guideline; Chiropractic
Dr. Alex Jimenez’s Insight
Headache, or head pain, including migraine and other types of headaches, is one of the most common types of pain reported among the general population. These may occur on one or both sides of the head, can be isolated to a specific location or they may radiate across the head from one point. While headache symptoms can vary depending on the type of head pain as well as due to the source of the health issue, headaches are considered to be a general complaint regardless of their severity and form. Headache, or head pain, may occur as a result of spinal misalignment, or subluxation, along the length of the spine. Through the use of spinal adjustments and manual manipulations, chiropractic care can safely and effectively realign the spine, reducing stress and pressure on the surrounding structures of the spine, to ultimately help improve migraine headache pain symptoms as well as overall health and wellness.
Headache is a common experience in adults. Recurring headaches negatively impact family life, social activity, and work capacity.[1,2] Worldwide, according to the World Health Organization, migraine alone is 19th among all causes of years lived with disability. Headache is third among reasons for seeking chiropractic care in North America.[3]
Accurate diagnosis is key to management and treatment, and a wide range of headache types are described in the International Classification of Headache Disorders 2 (International Headache Society [IHS]).[4] The categories are intended for clinical as well as research use. The most common headaches, tension-type and migraine, are considered primary headaches that are episodic or chronic in nature. Episodic migraine or tension-type headaches occur fewer than 15 days per month, whereas chronic headaches occur more than 15 days per month for at least 3 (migraine) or 6 months (tension-type headache).[4] Secondary headaches are attributed to underlying clinical problems in the head or neck that may also be episodic or chronic. Cervicogenic headaches are secondary headaches commonly treated by chiropractors and involve pain referred from a source in the neck and perceived in 1 or more regions of the head. The IHS recognizes cervicogenic headache as a distinct disorder,[4] and evidence that headache can be attributed to a neck disorder or lesion based on history and clinical features (history of neck trauma, mechanical exacerbation of pain, reduced cervical range of motion, and focal neck tenderness, excluding myofascial pain alone) is relevant to diagnosis but is not without controversy in the literature.[4,5] When myofascial pain alone is the cause, the patient should be managed as having tension-type headaches.[4]
Treatment modalities typically used by chiropractors to care for patients with headaches include spinal manipulation, mobilization, device-assisted spinal manipulation, education about modifiable lifestyle factors, physical therapy modalities, heat/ice, massage, advanced soft tissue therapies such as trigger point therapy, and strengthening and stretching exercises. There is a growing expectation for health professions, including chiropractic, to adopt and use research-based knowledge, taking sufficient account of the quality of available research evidence to inform clinical practice. As a result, the purpose of the Canadian Chiropractic Association (CCA) and the Canadian Federation of Chiropractic Regulatory and Educational Accrediting Boards (Federation) Clinical Practice Guidelines Project is to develop guidelines for practice based on available evidence. The purpose of this manuscript is to provide evidence-informed practice recommendations for the chiropractic treatment of headache in adults.
Methods
The Guidelines Development Committee (GDC) planned for and adapted systematic processes for literature searching, screening, review, analysis, and interpretation. Methods are consistent with criteria proposed by the “Appraisal of Guidelines Research and Evaluation” collaboration (www.agreecollaboration.org). This guideline is a supportive tool for practitioners. It is not intended as a standard of care. The guideline links available published evidence to clinical practice and is only 1 component of an evidence-informed approach to patient care.
Data Sources and Searches
Systematic search and evaluation of the treatment literature were conducted using methods recommended by The Cochrane Collaboration Back Review Group[6] and Oxman and Guyatt.[7] The search strategy was developed in MEDLINE by exploring MeSH terms related to chiropractic and specific interventions and later modified for other databases. The literature search strategy was intentionally broad. Chiropractic treatment was defined as including the most common therapies used by practitioners and was not restricted to treatment modalities delivered only by chiropractors. A wide net was cast to include treatments that may be administered in chiropractic care as well as those that could also be delivered in the context of care by other health care professionals in a specific research study (Appendix A). Spinal manipulation was defined as a high-velocity low-amplitude thrust delivered to the spine. Excluded therapies included invasive analgesic or neurostimulation procedures, pharmacotherapy, injections of botulinum toxin, cognitive or behavioral therapies, and acupuncture.
Literature searches were completed from April to May 2006, updated in 2007 (phase 1), and updated again in August 2009 (phase 2). Databases searched included MEDLINE; EMBASE; Allied and Complementary Medicine; the Cumulative Index to Nursing and Allied Health Literature; Manual, Alternative, and Natural Therapy Index System; Alt HealthWatch; Index to Chiropractic Literature; and the Cochrane Library (Appendix A). Searches included articles published in English or with English abstracts. The search strategy was limited to adults (≥18 years); although research studies with subject inclusion criteria encompassing a broad range of ages, such as adults and adolescents, were retrieved using the search strategy. Reference lists provided in systematic reviews (SRs) were also reviewed by the GDC to minimize relevant articles from being missed.
Evidence Selection Criteria
Search results were screened electronically, and multi-stage screening was applied (Appendix B): stage 1A (title), 1B (abstract); stage 2A (full text), 2B (full text-methodology, relevance); and stage 3 (full text-final GDC screening as clinical content experts). Duplicate citations were removed, and relevant articles were retrieved as electronic and/or hard copies for detailed analysis. Different assessors, using the same criteria, completed the literature screens in 2007 and 2009 due to the time span between searches.
Only controlled clinical trials (CCTs); randomized, controlled trials (RCTs); and systematic reviews (SRs) were selected as the evidence base for this guideline consistent with current standards for interpreting clinical findings. The GDC did not rate observational studies, case series, or case reports because of their uncontrolled nature and probable low methodological quality vs CCTs. This approach is consistent with updated methods for SRs published by the Cochrane Back Review Group.[8] If multiple SRs were published by the same authors on a given topic, only the most recent publication was counted and used for evidence synthesis. Systematic reviews of SRs were also excluded to avoid double counting of research results.
Literature Assessment and Interpretation
Quality ratings of CCTs or RCTs included 11 criteria answered by “yes (score 1)” or “no (score 0)/do not know (score 0)” (Table 1). The GDC documented 2 additional criteria of interest: (1) researchers’ use of IHS diagnostic criteria for subject enrollment and (2) evaluation of side effects (Table 1, columns L and M). Use of IHS criteria[4] was relevant to this Clinical Practice Guideline (CPG) process to confirm diagnostic specificity within and across research studies. Studies were excluded if IHS diagnostic criteria were not applied by the researchers for subject inclusion into a study (Appendix C); and if before 2004, before cervicogenic headache was included in the IHS classification, the diagnostic criteria of the Cervicogenic Headache International Study Group[9] were not used. Side effects were reviewed as a proxy for potential risk(s) with treatment. No weighting factor(s) was applied to individual criteria, and possible quality ratings ranged from 0 to 11. Both blinding of subjects and care providers were rated in the research articles by the GDC, since these items are listed in the quality rating tool.[6] The GDC’s methods did not adapt or alter the rating tool. The rationale for this approach was that certain treatment modalities (eg, transcutaneous electrical nerve stimulation [TENS], ultrasound) and trial designs may achieve patient and/or practitioner blinding.[10] The GDC did not limit the evaluation of these benchmarks of quality if indeed they were reported in clinical studies for the treatment of headache disorders. The GDC also considered it outside their scope of expertise to modify, without validation, a widely used rating tool used to assess the clinical literature.[6] New research tools for the analysis and rating of the manual therapy literature, however, are urgently needed and are noted as an area for future research in the discussion section below.
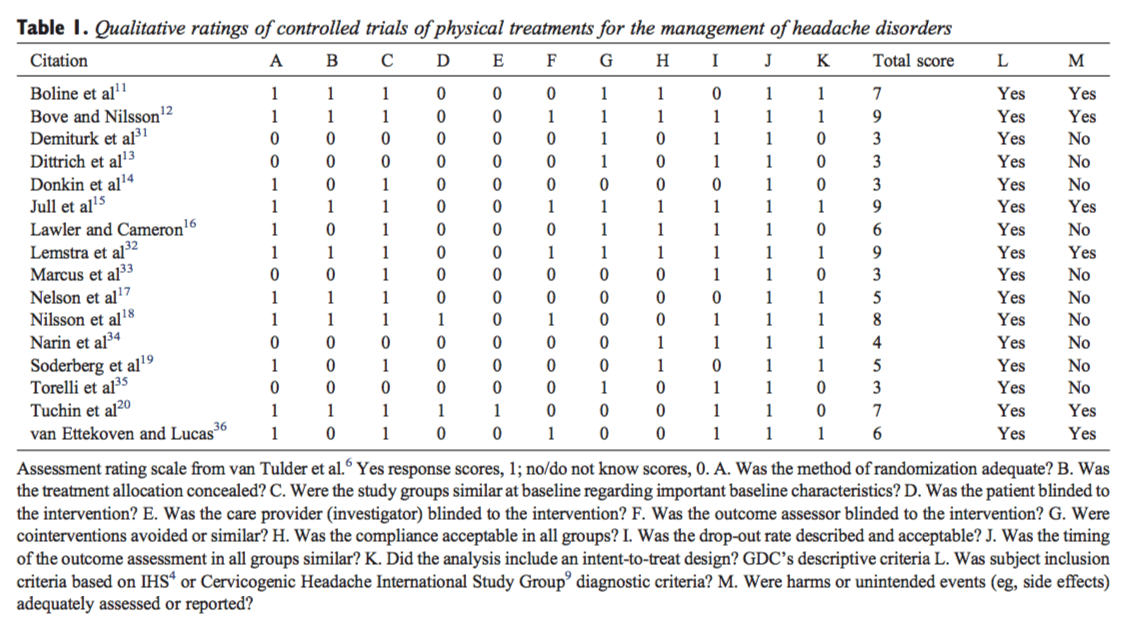
Literature assessors were project contributors separate from the GDC and were unblinded as to study authors, institutions, and source journals. Three members of the GDC (MD, RR, and LS) corroborated quality rating methods by completing quality assessments on a random subset of 10 articles.[11-20] A high level of agreement was confirmed across quality ratings. Complete agreement on all items was achieved for 5 studies: in 10 of 11 items for 4 studies and 8 of 11 items for the 1 remaining study. All discrepancies were easily resolved through discussion and consensus by the GDC (Table 1). Due to heterogeneity of research methods across trials, no meta-analysis or statistical pooling of trial results was done. Trials scoring more than half of the total possible rating (ie, ≥6) were considered high quality. Trials scoring 0 through 5 were considered low quality. Studies with major methodological flaws or investigating specialized treatment techniques were excluded (eg, treatment not considered relevant by the GDC for the chiropractic care of patients with headache; Appendix Table 3).
Quality rating of SRs included 9 criteria answered by yes (score 1) or no (score 0)/do not know (score 0) and a qualitative response for item J “no flaws,” “minor flaws,” or “major flaws” (Table 2). Possible ratings ranged from 0 to 9. The determination of overall scientific quality of SRs with major flaws, minor flaws, or no flaws, as listed in column J (Table 2), was based on the literature raters’ answers to the previous 9 items. The following parameters were used to derive the overall scientific quality of a SR: if the no/do not know response was used, an SR was likely to have minor flaws at best. However, if “No” was used on items B, D, F, or H, the review was likely to have major flaws.[21] Systematic reviews scoring more than half of the total possible rating (ie, ≥5) with no or minor flaws were rated as high quality. Systematic reviews scoring 4 or less and/or with major flaws were excluded.
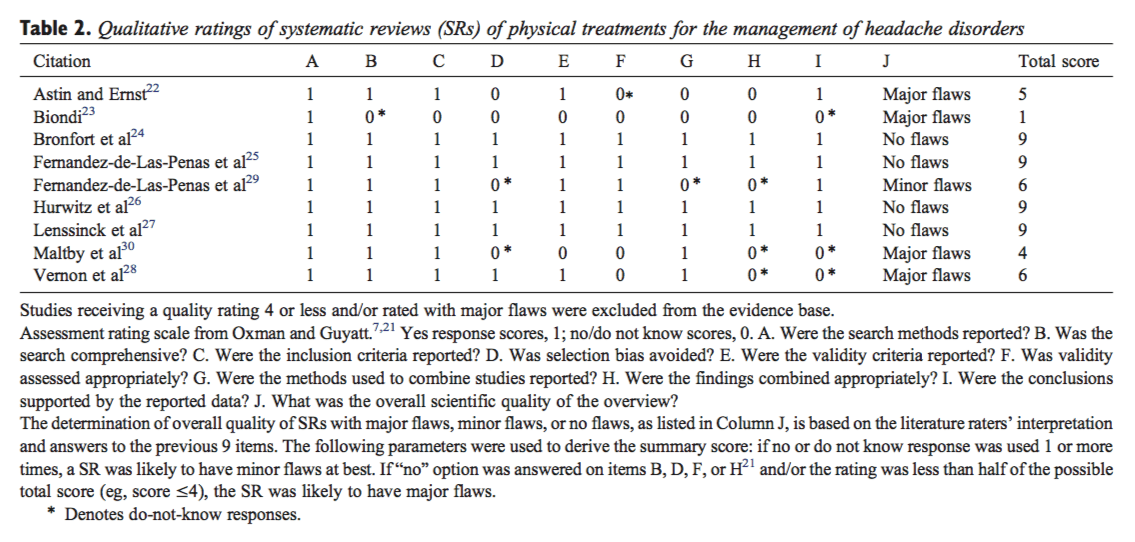
Reviews were defined as systematic if they included an explicit and repeatable method for searching and analyzing the literature and if inclusion and exclusion criteria for studies were described. Methods, inclusion criteria, methods for rating study quality, characteristics of included studies, methods for synthesizing data, and results were evaluated. Raters achieved complete agreement for all rating items for 7 SRs[22-28] and for 7 of 9 items for the 2 additional SRs.[29,30] The discrepancies were deemed minor and easily resolved through GDC review and consensus (Table 2).
Developing Recommendations for Practice
The GDC interpreted the evidence relevant to chiropractic treatment of headache patients. A detailed summary of the relevant articles will be posted to the CCA/Federation Clinical Practice Guidelines Project web site.
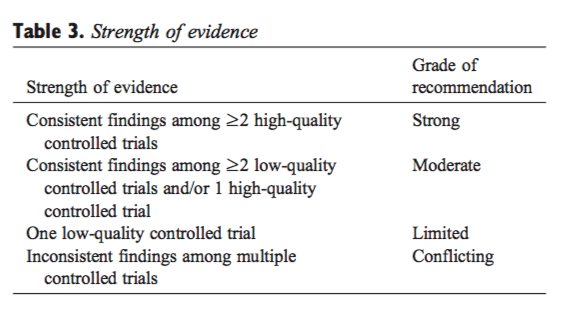
Randomized, controlled trials and their findings were appraised to inform treatment recommendations. To assign an overall strength of evidence (strong, moderate, limited, conflicting, or no evidence),[6] the GDC considered the number, quality, and consistency of research results (Table 3). Strong evidence was considered only when multiple high-quality RCTs corroborated the findings of other researchers in other settings. Only high-quality SRs were appraised in relation to the body of evidence and to inform treatment recommendations. The GDC considered treatment modalities to have proven benefit(s) when supported by a minimum of moderate level of evidence.
Recommendations for practice were developed in collaborative working group meetings.
Results
Literature
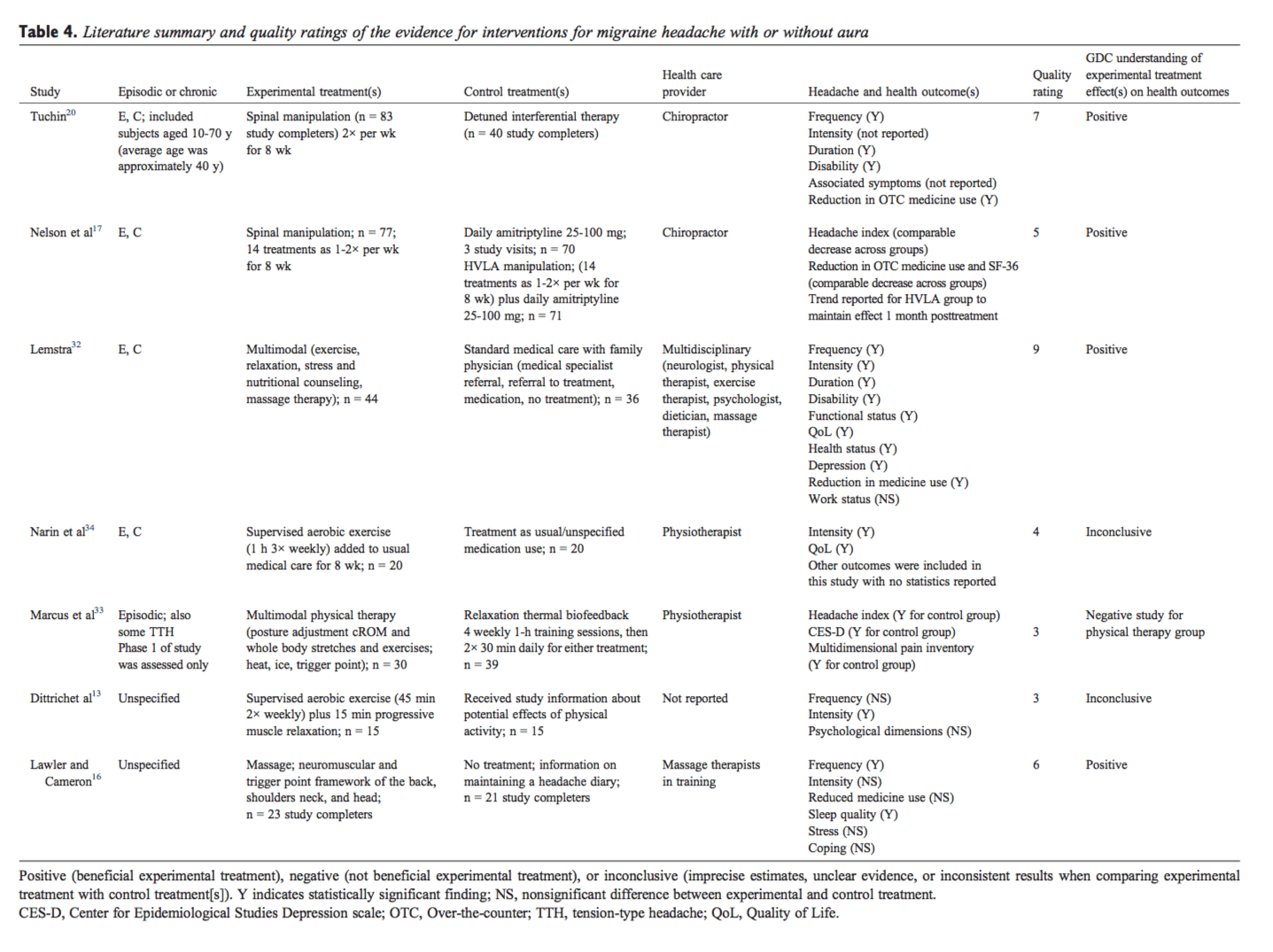
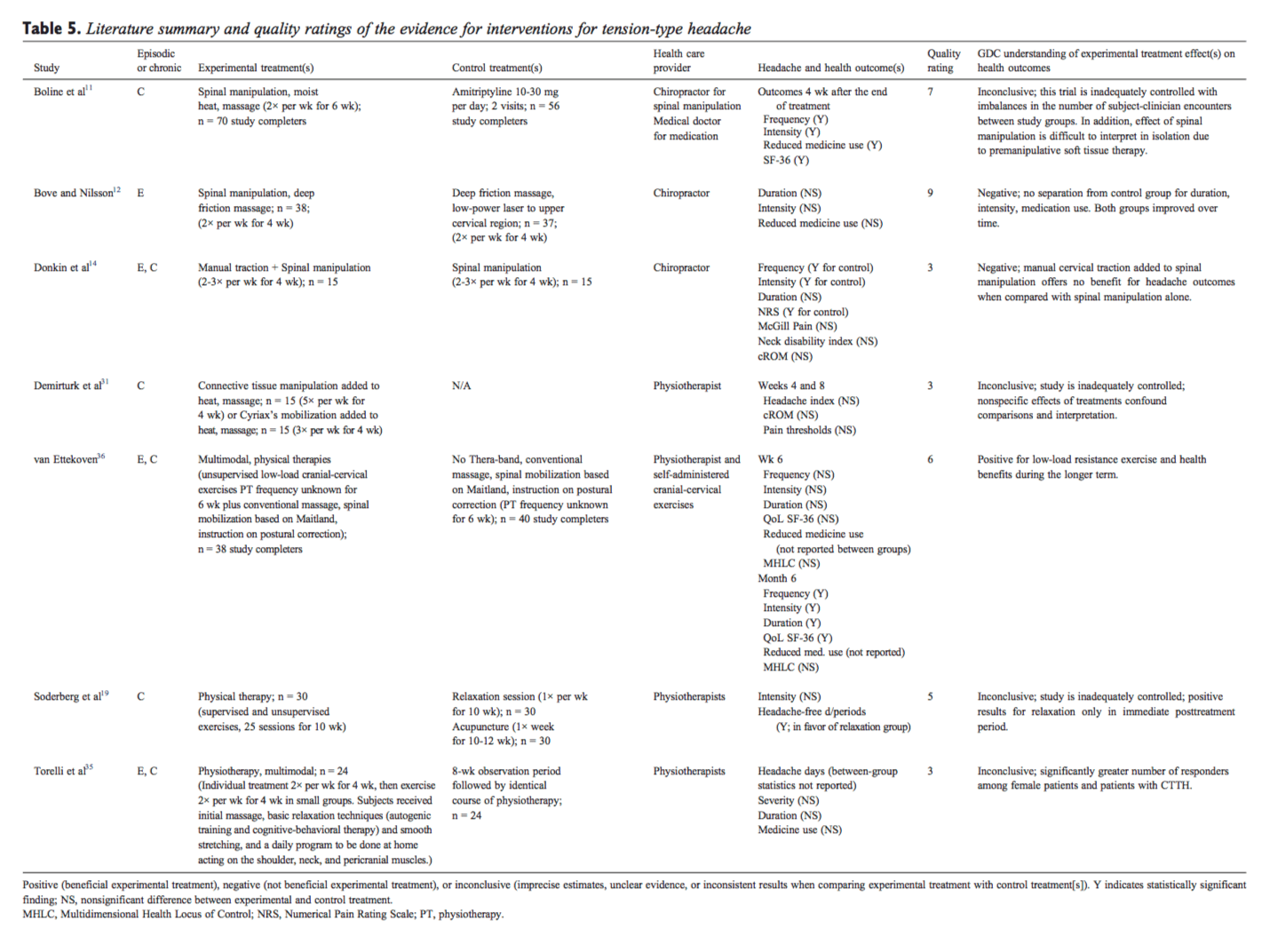
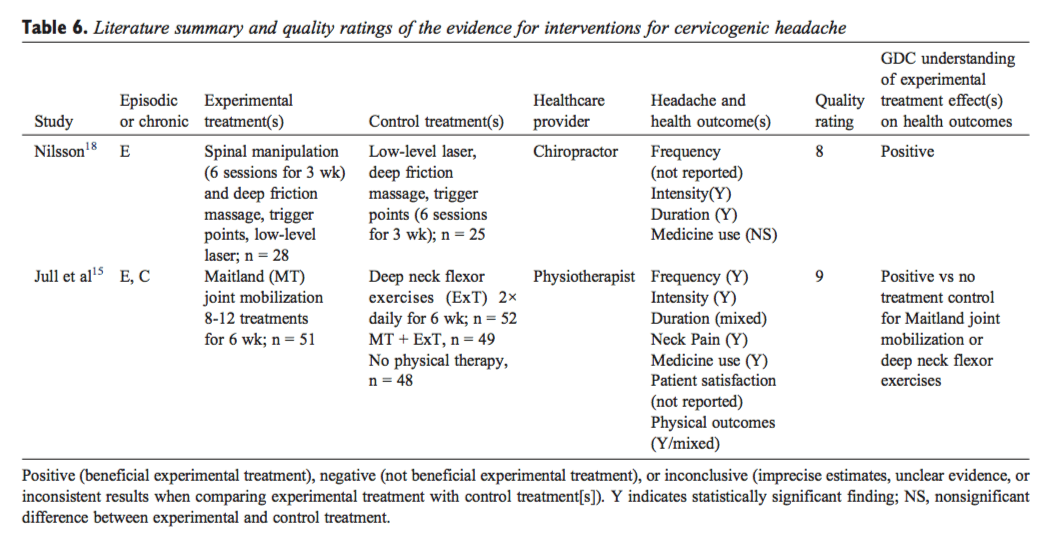
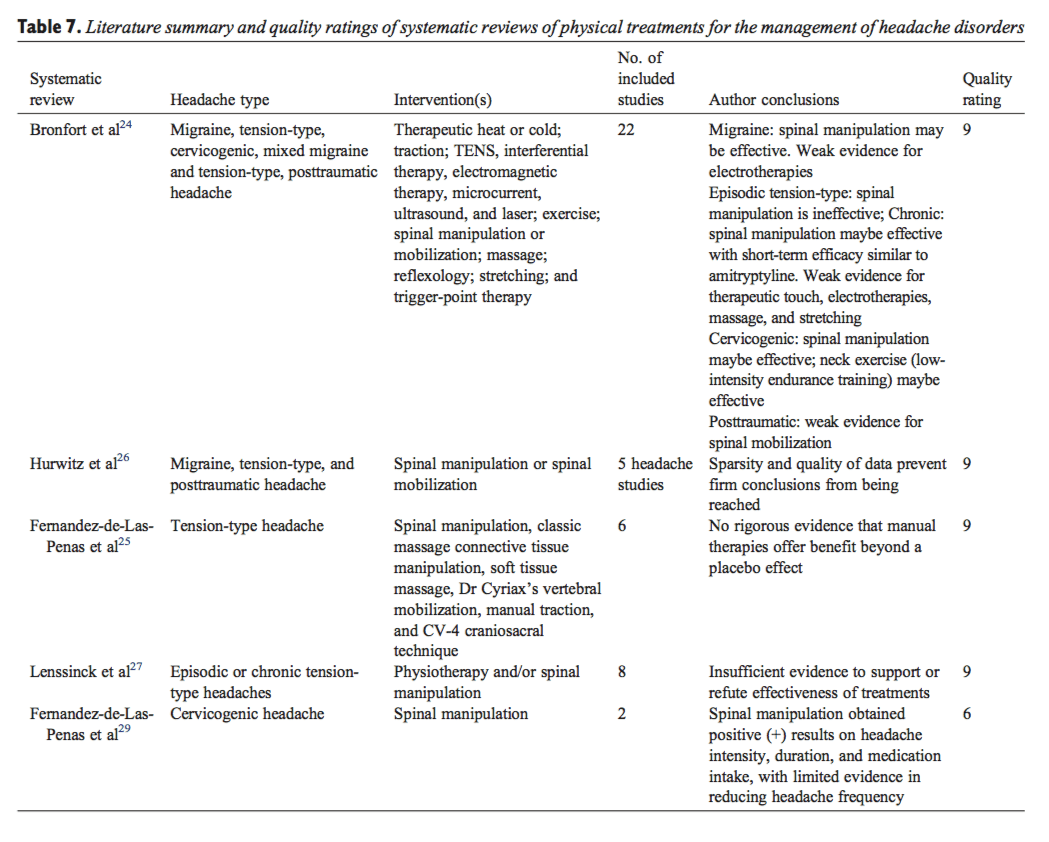
From the literature searches, initially 6206 citations were identified. Twenty-one articles met final criteria for inclusion and were considered in developing practice recommendations (16 CCTs/RCTs[11-20,31-36] and 5 SRs[24-27,29]). Quality ratings of the included articles are provided in Tables 1 and 2. Appendix Table 3 lists articles excluded in final screening by the GDC and reason(s) for their exclusion. Absence of subject and practitioner blinding and unsatisfactory descriptions of cointerventions were commonly identified methodological limitations of the controlled trials. Headache types evaluated in these trials included migraine (Table 4), tension-type headache (Table 5), and cervicogenic headache (Table 6). Consequently, only these headache types are represented by the evidence and practice recommendations in this CPG. Evidence summaries of SRs are provided in Table 7.
Practice Recommendations: Treatment of Migraine
- Spinal manipulation is recommended for the management of patients with episodic or chronic migraine with or without aura. This recommendation is based on studies that used a treatment frequency 1 to 2 times per week for 8 weeks (evidence level, moderate). One high-quality RCT,[20] 1 low-quality RCT,[17] and 1 high- quality SR[24] support the use of spinal manipulation for patients with episodic or chronic migraine (Tables 4 and 7).
- Weekly massage therapy is recommended for reducing episodic migraine frequency and for improving affective symptoms potentially linked to headache pain (evidence level, moderate). One high-quality RCT[16] supports this practice recommendation (Table 4). Researchers used a 45-minute massage with focus on neuromuscular and trigger point framework of the back, shoulder, neck, and head.
- Multimodal multidisciplinary care (exercise, relaxation, stress and nutritional counseling, massage therapy) is recommended for the management of patients with episodic or chronic migraine. Refer as appropriate (evidence level, moderate). One high-quality RCT[32] supports the effectiveness of multi-modal multidisciplinary intervention for migraine (Table 4). The intervention prioritizes a general management approach consisting of exercise, education, lifestyle change, and self-management.
- There are insufficient clinical data to recommend for or against the use of exercise alone or exercise combined with multimodal physical therapies for the management of patients with episodic or chronic migraine (aerobic exercise, cervical range of motion [cROM], or whole body stretching). Three low-quality CCTs[13,33,34] contribute to this conclusion (Table 4).
Practice Recommendations: Tension-Type Headache
- Low-load craniocervical mobilization (eg, Thera-Band, Resistive Exercise Systems; Hygenic Corporation, Akron, OH) is recommended for longer term (eg, 6 months) management of patients with episodic or chronic tension-type headaches (evidence level, moderate). One high-quality RCT[36] showed that low-load mobilization significantly reduced symptoms of tension-type headaches for patients during the longer term (Table 5).
- Spinal manipulation cannot be recommended for the management of patients with episodic tension-type headache (evidence level, moderate). There is moderate-level evidence that spinal manipulation after premanipulative soft tissue therapy provides no additional benefit for patients with tension-type headaches. One high-quality RCT[12] (Table 5) and observations reported in 4 SRs[24-27] (Table 7) suggest no benefit of spinal manipulation for patients with episodic tension-type headaches.
- A recommendation cannot be made for or against the use of spinal manipulation (2 times per week for 6 weeks) for patients with chronic tension-type headache. Authors of 1 RCT[11] rated as high quality by the quality assessment tool[6] (Table 1), and summaries of this study in 2 SRs[24,26] suggest that spinal manipulation may be effective for chronic tension-type headache. However, the GDC considers the RCT[11] difficult to interpret and inconclusive (Table 5). The trial is inadequately controlled with imbalances in the number of subject-clinician encounters between study groups (eg, 12 visits for subjects in the soft tissue therapy plus spinal manipulation group vs 2 visits for subjects in the amitriptyline group). There is no way of knowing whether a comparable level of personal attention for subjects in the amitriptyline group may have impacted the study outcomes. These considerations and interpretations from 2 other SRs[25,27]contribute to this conclusion (Table 7).
- There is insufficient evidence to recommend for or against the use of manual traction, connective tissue manipulation, Cyriax’s mobilization, or exercise/ physical training for patients with episodic or chronic tension-type headache. Three low-quality inconclusive studies[19,31,35] (Table 5), 1 low-quality negative RCT,[14] and 1 SR[25] contribute to this conclusion (Table 7).
Practice Recommendations: Cervicogenic Headache
- Spinal manipulation is recommended for the management of patients with cervicogenic headache. This recommendation is based on 1 study that used a treatment frequency of 2 times per week for 3 weeks (evidence level, moderate). In a high-quality RCT, Nilsson et al[18] (Table 6) showed a significantly positive effect of high-velocity, low-amplitude spinal manipulation for patients with cervicogenic headache. Evidence synthesis from 2 SRs[24,29] (Table 7) supports this practice recommendation.
- Joint mobilization is recommended for the management of patients with cervicogenic headache (evidence level, moderate). Jull et al[15] examined the effects of Maitland joint mobilization 8 to 12 treatments for 6 weeks in a high-quality RCT (Table 6). Mobilization followed typical clinical practice, in which the choice of low-velocity and high-velocity techniques was based on initial and progressive assessments of patients’ cervical joint dysfunction. Beneficial effects were reported for headache frequency, intensity, as well as neck pain and disability. Evidence synthesis from 2 SRs[24,29] (Table 7) supports this practice recommendation.
- Deep neck flexor exercises are recommended for the management of patients with cervicogenic headache (evidence level, moderate). This recommendation is based on a study of 2 times daily for 6 weeks. There is no consistently additive benefit of combining deep neck flexor exercises and joint mobilization for cervicogenic headache. One high-quality RCT[15] (Table 6) and observations provided in 2 SRs[24,29] (Table 7) support this practice recommendation.
Safety
Practitioners select treatment modalities in conjunction with all available clinical information for a given patient. Of the 16 CCTs/RCTS[11-20,31-36] included in the body of evidence for this CPG, only 6 studies[11,12,15,20,32,36] adequately assessed or discussed patient side effects or safety parameters (Table 1, column M). Overall, reported risks were low. Three of the trials reported safety information for spinal manipulation.[11,12,20] Boline et al[11] reported that 4.3% of subjects experienced neck stiffness after initial spinal manipulation that disappeared for all cases after the first 2 weeks of treatment. Soreness or increase in headaches after spinal manipulation (n = 2) were reasons for treatment discontinuation cited by Tuchin et al.[20] No side effects were experienced by any subjects studied by Bove et al[12] using spinal manipulation for the treatment of episodic tension-type headache. Treatment trials to evaluate efficacy outcomes may not enroll adequate numbers of subjects to assess the incidence of rare adverse events. Other research methods are required to develop a full understanding of the balance between benefits and risks.
Discussion
Spinal manipulation and other manual therapies commonly used in chiropractic have been studied in several CCTs that are heterogeneous in subject enrollment, design, and overall quality. Patient and headache types systematically represented in the evidence base are migraine, tension-type headaches, and cervicogenic headache. The primary health status outcomes reported are typically headache frequency, intensity, duration, and quality-of-life measures. The evidence is no greater than a moderate level at this time.
The evidence supports the use of spinal manipulation for the chiropractic management of patients with migraine or cervicogenic headaches but not tension-type headaches. For migraine, multidisciplinary care using weekly 45-minute massage therapy and multimodal care (exercise, relaxation, and stress and nutritional counseling) may also be effective. Alternatively, joint mobilization or deep neck flexor exercises are recommended for improving symptoms of cervicogenic headache. There appears to be no consistently additive benefit of combining joint mobilization and deep neck flexor exercises for patients with cervicogenic headache. Moderate evidence support the use of low-load craniocervical mobilization for longer term management of tension-type headaches.
Limitations
Shortcomings for this guideline include the quantity and quality of supporting evidence found during the searches. No recent adequately controlled high-quality research studies with reproducible clinical findings have been published for the chiropractic care of headache patients. Studies are needed to further our understanding of specific manual therapies in isolation or in well-controlled combinations for the treatment of migraine, tension-type headache, cervicogenic headache, or other headache types presenting to clinicians (eg, cluster, posttraumatic head- ache). Another shortcoming of this literature synthesis is the reliance on published research studies with small sample sizes (Tables 4-6), short-term treatment paradigms, and follow-up periods. Well-designed clinical trials with sufficient numbers of subjects, longer term treatments, and follow-up periods need to be funded to advance chiropractic care, and spinal manipulation in particular, for the management of patients with headache disorders. As with any literature review and clinical practice guideline, foundational information and published literature are evolving. Studies that may have informed this work may have been published after the conclusion of this study.[37-39]
Considerations for Future Research
The GDC consensus is that there is a need for further chiropractic studies with patients with headache disorders.
- More high-quality clinical research is needed. Future research requires study designs using active comparators and nontreatment and/or placebo group(s) to enhance the evidence base for patient care. Patient blinding to physical interventions to manage expectancy results is needed and has been explored by researchers in chiropractic for other pain conditions.[10] The lack of systematically reported studies presents a practical challenge for generating evidence-based treatment recommendations. All future studies should be structured using systematic validated methods (eg, Consolidated Standards of Reporting Trials [CONSORT] and Transparent Reporting of Evaluations with Non-randomized Designs [TREND]).
- Systematic reporting of safety data is needed in chiropractic research. All clinical trials must collect and report on potential side effects or harms even if none are observed.
- Develop novel quantitative tools for evaluating manual therapy research. Blinding serves to control expectancy effects and nonspecific effects of subject-provider interactions across study groups. It is typically not possible to blind subjects and providers in efficacy studies of manual therapies. Despite inherent limitations, both blinding of subjects and care providers were rated in the research articles by the GDC, since these items are included in high-quality rating instruments.[6] Advanced research tools for analyzing and subsequent rating of the manual therapy literature are urgently needed.
- To advance research on functional outcomes in the chiropractic care of headache. This guideline identified that headache studies use a variable range of measures in evaluating the effect of treatment on health outcomes. Headache frequency, intensity, and duration are the most consistently used outcomes (Tables 4-6). Serious efforts are needed to include validated patient-centered outcome measures in chiropractic research that are congruent with improvements in daily living and resumption of meaningful routines.
- Cost-effectiveness. No research studies were retrieved on cost-effectiveness of spinal manipulation for the treatment of headache disorders. Future clinical trials of spinal manipulation should evaluate cost-effectiveness.
Other research methods are required to develop a full understanding of the balance between benefits and risks. This CPG does not provide a review of all chiropractic treatments. Any omissions reflect gaps in the clinical literature. The type, frequency, dosage, and duration of treatment(s) should be based on guideline recommendations, clinical experience, and knowledge of the patient until higher levels of evidence are available.
Conclusions
There is a baseline of evidence to support chiropractic care, including spinal manipulation, for the management of migraine and cervicogenic headaches. The type, frequency, dosage, and duration of treatment(s) should be based on guideline recommendations, clinical experience, and knowledge of the patient. Evidence for the use of spinal manipulation as an isolated intervention for patients with tension-type headache remains equivocal. More research is needed.
Practice guidelines link the best available evidence to good clinical practice and are only 1 component of an evidence-informed approach to providing good care. This guideline is intended to be a resource for the delivery of chiropractic care for patients with headache. It is a “living document” and subject to revision with the emergence of new data. Furthermore, it is not a substitute for a practitioner’s clinical experience and expertise. This document is not intended to serve as a standard of care. Rather, the guideline attests to the commitment of the profession to advance evidence-based practice through engaging a knowledge exchange and transfer process to support the movement of research knowledge into practice.
Practical Applications
- This guideline is a resource for the delivery of chiropractic care for patients with headache.
- Spinal manipulation is recommended for the management of patients with migraine or cervicogenic headaches.
- Multimodal multidisciplinary interventions including massage may benefit patients with migraine.
- Joint mobilization or deep neck flexor exercises may improve symptoms of cervicogenic headache.
- Low-load craniocervical mobilization may improve tension-type headaches.
Acknowledgements
The authors thank the following for input on this guideline: Ron Brady, DC; Grayden Bridge, DC; H James Duncan; Wanda Lee MacPhee, DC; Keith Thomson, DC, ND; Dean Wright, DC; and Peter Waite (Members of the Clinical Practice Guidelines Task Force). The authors thank the following for assistance with the Phase I literature search assessment: Simon Dagenais, DC, PhD; and Thor Eglinton, MSc, RN. The authors thank the following for assistance with the Phase II additional literature search and evidence rating: Seema Bhatt, PhD; Mary-Doug Wright, MLS. The authors thank Karin Sorra, PhD for assistance with literature searches, evidence rating, and editorial support.
Funding Sources and Potential Conflicts of Interest
Funding was provided by the CCA, Canadian Chiropractic Protective Association, and provincial chiropractic contributions from all provinces except British Columbia. This work was sponsored by The CCA and the Federation. No conflicts of interest were reported for this study.
In conclusion, headache is one of the most common reasons people seek medical attention. Although many healthcare professionals can treat headaches, chiropractic care is a well-known alternative treatment option frequently used to treat a variety of health issues, including several types of headaches. According to the article above, evidence suggests that chiropractic care, including spinal adjustments and manual manipulations, can improve headache and migraine. Information referenced from the National Center for Biotechnology Information (NCBI). The scope of our information is limited to chiropractic as well as to spinal injuries and conditions. To discuss the subject matter, please feel free to ask Dr. Jimenez or contact us at 915-850-0900 .
Curated by Dr. Alex Jimenez
Additional Topics: Back Pain
According to statistics, approximately 80% of people will experience symptoms of back pain at least once throughout their lifetimes. Back pain is a common complaint which can result due to a variety of injuries and/or conditions. Often times, the natural degeneration of the spine with age can cause back pain. Herniated discs occur when the soft, gel-like center of an intervertebral disc pushes through a tear in its surrounding, outer ring of cartilage, compressing and irritating the nerve roots. Disc herniations most commonly occur along the lower back, or lumbar spine, but they may also occur along the cervical spine, or neck. The impingement of the nerves found in the low back due to injury and/or an aggravated condition can lead to symptoms of sciatica.

EXTRA IMPORTANT TOPIC: Neck Pain Treatment El Paso, TX Chiropractor
MORE TOPICS: EXTRA EXTRA: El Paso, Tx | Athletes
[/et_pb_text][et_pb_accordion _builder_version=”3.0.106″][et_pb_accordion_item _builder_version=”3.0.106″ title=”Blank” use_background_color_gradient=”off” background_color_gradient_start=”#2b87da” background_color_gradient_end=”#29c4a9″ background_color_gradient_type=”linear” background_color_gradient_direction=”180deg” background_color_gradient_direction_radial=”center” background_color_gradient_start_position=”0%” background_color_gradient_end_position=”100%” background_color_gradient_overlays_image=”off” parallax=”off” parallax_method=”on” background_size=”cover” background_position=”center” background_repeat=”no-repeat” background_blend=”normal” allow_player_pause=”off” background_video_pause_outside_viewport=”on” text_shadow_style=”none” box_shadow_style=”none” custom_css_main_element=”display:none;” /][et_pb_accordion_item _builder_version=”3.0.106″ title=”References” use_background_color_gradient=”off” background_color_gradient_start=”#2b87da” background_color_gradient_end=”#29c4a9″ background_color_gradient_type=”linear” background_color_gradient_direction=”180deg” background_color_gradient_direction_radial=”center” background_color_gradient_start_position=”0%” background_color_gradient_end_position=”100%” background_color_gradient_overlays_image=”off” parallax=”off” parallax_method=”on” background_size=”cover” background_position=”center” background_repeat=”no-repeat” background_blend=”normal” allow_player_pause=”off” background_video_pause_outside_viewport=”on” text_shadow_style=”none” box_shadow_style=”none”]
1. Robbins MS, Lipton RB. The epidemiology of primary headache disorders. Semin Neurol 2010;30:107-19.
2. Stovner LJ, Andree C. Prevalence of headache in Europe: a review for the Eurolight project. J Headache Pain Aug 2010; 11:289-99.
3. Coulter ID, Hurwitz EL, Adams AH, Genovese BJ, Hays R, Shekelle PG. Patients using chiropractors in North America: who are they, and why are they in chiropractic care? Spine (Phila Pa 1976) 2002;27(3):291-6 [discussion 297-98].
4. International Headache Society. The International Classifi- cation of Headache Disorders, 2nd ed. Cephalalgia 2004;24: 9-160 (Suppl 1).
5. Bogduk N, Govind J. Cervicogenic headache: an assessment of the evidence on clinical diagnosis, invasive tests, and treatment. Lancet Neurol 2009;8:959-68.
6. van Tulder M, Furlan A, Bombardier C, Bouter L. Updated method guidelines for systematic reviews in the cochrane collaboration back review group. Spine (Phila Pa 1976) 2003; 28:1290-9.
7. Oxman AD, Guyatt GH. Validation of an index of the quality of review articles. J Clin Epidemiol 1991;44:1271-8.
8. Furlan AD, Pennick V, Bombardier C, van Tulder M. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine (Phila Pa 1976) 2009; 34:1929-41.
9. Sjaastad O, Fredriksen TA, Pfaffenrath V. Cervicogenic headache: diagnostic criteria. The Cervicogenic Headache International Study Group. Headache 1998;38:442-5.
10. Hawk C, Long CR, Reiter R, Davis CS, Cambron JA, Evans R. Issues in planning a placebo-controlled trial of manual methods: results of a pilot study. J Altern Complement Med 2002;8:21-32.
11. Boline PD, Kassak K, Bronfort G, Nelson C, Anderson AV. Spinal manipulation vs. amitriptyline for the treatment of chronic tension-type headaches: a randomized clinical trial. J Manipulative Physiol Ther 1995;18:148-54.
12. Bove G, Nilsson N. Spinal manipulation in the treatment of episodic tension-type headache: a randomized controlled trial. JAMA 1998;280:1576-9.
13. Dittrich SM, Gunther V, Franz G, Burtscher M, Holzner B, Kopp M. Aerobic exercise with relaxation: influence on pain and psychological well-being in female migraine patients. Clin J Sport Med 2008;18:363-5.
14. Donkin RD, Parkin-Smith GF, Gomes N. Possible effect of chiropractic manipulation and combined manual traction and manipulation on tension-type headache: a pilot study. J Neuromusculoskeletal Systen 2002;10:89-97.
15. Jull G, Trott P, Potter H, et al. A randomized controlled trial of exercise and manipulative therapy for cervicogenic headache. Spine (Phila Pa 1976) 2002;27:1835-43 [discussion 1843].
16. Lawler SP, Cameron LD. A randomized, controlled trial of massage therapy as a treatment for migraine. Ann Behav Med 2006;32:50-9.
17. Nelson CF, Bronfort G, Evans R, Boline P, Goldsmith C, Anderson AV. The efficacy of spinal manipulation, amitrip- tyline and the combination of both therapies for the prophylaxis of migraine headache. J Manipulative Physiol Ther 1998;21:511-9.
18. Nilsson N, Christensen HW, Hartvigsen J. The effect of spinal manipulation in the treatment of cervicogenic headache. J Manipulative Physiol Ther 1997;20:326-30.
19. Soderberg E, Carlsson J, Stener-Victorin E. Chronic tension- type headache treated with acupuncture, physical training and relaxation training. Between-group differences. Cephalalgia 2006;26:1320-9.
20. Tuchin PJ, Pollard H, Bonello R. A randomized controlled trial of chiropractic spinal manipulative therapy for migraine. J Manipulative Physiol Ther 2000;23:91-5.
21. Chou R, Huffman LH. Nonpharmacologic therapies for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med 2007;147: 492-504.
22. Astin JA, Ernst E. The effectiveness of spinal manipulation for the treatment of headache disorders: a systematic review of randomized clinical trials. Cephalalgia 2002;22:617-23.
23. Biondi DM. Physical treatments for headache: a structured review. Headache 2005;45:738-46.
24. Bronfort G, Nilsson N, Haas M, et al. Non-invasive physical treatments for chronic/recurrent headache. Cochrane Database Syst Rev 2004:CD001878.
25. Fernandez-de-Las-Penas C, Alonso-Blanco C, Cuadrado ML, Miangolarra JC, Barriga FJ, Pareja JA. Are manual therapies effective in reducing pain from tension-type headache?: a systematic review. Clin J Pain 2006;22:278-85.
26. Hurwitz EL, Aker PD, Adams AH, Meeker WC, Shekelle PG. Manipulation and mobilization of the cervical spine. A systematic review of the literature. Spine (Phila Pa 1976) 1996;21:1746-59.
27. Lenssinck ML, Damen L, Verhagen AP, Berger MY, Passchier J, Koes BW. The effectiveness of physiotherapy and manipulation in patients with tension-type headache: a systematic review. Pain 2004;112:381-8.
28. Vernon H, McDermaid CS, Hagino C. Systematic review of randomized clinical trials of complementary/alternative ther- apies in the treatment of tension-type and cervicogenic headache. Complement Ther Med 1999;7:142-55.
29. Fernandez-de-Las-Penas C, Alonso-Blanco C, Cuadrado ML, Pareja JA. Spinal manipulative therapy in the management of cervicogenic headache. Headache 2005;45:1260-3.
30. Maltby JK, Harrison DD, Harrison D, Betz J, Ferrantelli JR, Clum GW. Frequency and duration of chiropractic care for headaches, neck and upper back pain. J Vertebr Subluxat Res 2008;2008:1-12.
31. Demirturk F, Akarcali I, Akbayrak T, Cita I, Inan L. Results of two different manual therapy techniques in chronic tension- type headache. Pain Clin 2002;14:121-8.
32. Lemstra M, Stewart B, Olszynski WP. Effectiveness of multidisciplinary intervention in the treatment of migraine: a randomized clinical trial. Headache 2002;42:845-54.
33. Marcus DA, Scharff L, Mercer S, Turk DC. Nonpharmaco- logical treatment for migraine: incremental utility of physical therapy with relaxation and thermal biofeedback. Cephalalgia 1998;18:266-72.
34. Narin SO, Pinar L, Erbas D, Ozturk V, Idiman F. The effects of exercise and exercise-related changes in blood nitric oxide level on migraine headache. Clin Rehabil 2003;17:624-30.
35. Torelli P, Jensen R, Olesen J. Physiotherapy for tension-type headache: a controlled study. Cephalalgia 2004;24:29-36.
36. van Ettekoven H, Lucas C. Efficacy of physiotherapy
including a craniocervical training programme for tension- type headache; a randomized clinical trial. Cephalalgia 2006; 26:983-91.
37. Vavrek D, Haas M, Peterson D. Physical examination and self-reported pain outcomes from a randomized trial on chronic cervicogenic headache. J Manipulative Physiol Ther 2010;33:338-48.
38. Haas M, Aickin M, Vavrek D. A preliminary path analysis of expectancy and patient-provider encounter in an open-label randomized controlled trial of spinal manipulation for cervicogenic headache. J Manipulative Physiol Ther 2010; 33:5-13.
39. Toro-Velasco C, Arroyo-Morales M, Fernández-de-Las- Peñas C, Cleland JA, Barrero-Hernández FJ. Short-term effects of manual therapy on heart rate variability, mood state, and pressure pain sensitivity in patients with chronic tension-type headache: a pilot study. J Manipulative Physiol Ther 2009;32:527-35.
40. Allais G, De Lorenzo C, Quirico PE, et al. Non-pharmaco- logical approaches to chronic headaches: transcutaneous electrical nerve stimulation, lasertherapy and acupuncture in transformed migraine treatment. Neurol Sci 2003;24(Suppl 2): S138-42.
41. Nilsson N. A randomized controlled trial of the effect of spinal manipulation in the treatment of cervicogenic head- ache. J Manipulative Physiol Ther 1995;18:435-40.
42. Annal N, Soundappan SV, Palaniappan KMC, Chadrasekar S. Introduction of transcutaneous, low-voltage, non-pulsatile direct current (DC) therapy for migraine and chronic headaches. A comparison with transcutaneous electrical nerve stimulation (TENS). Headache Q 1992;3:434-7.
43. Nilsson N, Christensen HW, Hartvigsen J. Lasting changes in passive range motion after spinal manipulation: a randomized, blind, controlled trial. J Manipulative Physiol Ther 1996;19: 165-8.
44. Anderson RE, Seniscal C. A comparison of selected osteopathic treatment and relaxation for tension-type head- aches. Headache 2006;46:1273-80.
45. Ouseley BR, Parkin-Smith GF. Possible effects of chiropractic spinal manipulation and mobilization in the treatment of chronic tension-type headache: a pilot study. Eur J Chiropr 2002;50:3-13.
46. Fernandez-de-las-Penas C, Fernandez-Carnero J, Plaza Fernandez A, Lomas-Vega R, Miangolarra-Page JC. Dorsal manipulation in whiplash injury treatment: a randomized controlled trial. J Whiplash Related Disorders 2004;3:55-72.
47. Parker GB, Pryor DS, Tupling H. Why does migraine improve during a clinical trial? Further results from a trial of cervical manipulation for migraine. Aust N Z J Med 1980; 10:192-8.
48. Parker GB, Tupling H, Pryor DS. A controlled trial of cervical manipulation of migraine. Aust N Z J Med 1978;8:589-93.
49. Foster KA, Liskin J, Cen S, et al. The Trager approach in the treatment of chronic headache: a pilot study. Altern Ther Health Med 2004;10:40-6.
50. Haas M, Groupp E, Aickin M, et al. Dose response for chiropractic care of chronic cervicogenic headache and associated neck pain: a randomized pilot study. J Manipula- tive Physiol Ther 2004;27:547-53.
51. Sjogren T, Nissinen KJ, Jarvenpaa SK, Ojanen MT, Vanharanta H, Malkia EA. Effects of a workplace physical exercise intervention on the intensity of headache and neck and shoulder symptoms and upper extremity muscular strength of office workers: a cluster randomized controlled cross-over trial. Pain 2005;116:119-28.
52. Hanten WP, Olson SL, Hodson JL, Imler VL, Knab VM, Magee JL. The effectiveness of CV-4 and resting position techniques on subjects with tension-type headaches. J Manual Manipulative Ther 1999;7:64-70.
53. Solomon S, Elkind A, Freitag F, Gallagher RM, Moore K, Swerdlow B, et al. Safety and effectiveness of cranial electrotherapy in the treatment of tension headache. Headache 1989;29:445-50.
54. Hall T, Chan HT, Christensen L, Odenthal B, Wells C, Robinson K. Efficacy of a C1-C2 self-sustained natural apophyseal glide (SNAG) in the management of cervicogenic headache. J Orthop Sports Phys Ther 2007;37:100-7.
55. Solomon S, Guglielmo KM. Treatment of headache by transcutaneous electrical stimulation. Headache 1985;25: 12-5.
56. Hoyt WH, Shaffer F, Bard DA, Benesler ES, Blankenhorn GD, Gray JH, et al. Osteopathic manipulation in the treatment of muscle-contraction headache. J Am Osteopath Assoc 1979;78:322-5.
57. Vernon H, Jansz G, Goldsmith CH, McDermaid C. A randomized, placebo-controlled clinical trial of chiropractic and medical prophylactic treatment of adults with tension-type headache: results from a stopped trial. J Manipulative Physiol Ther 2009;32:344-51.
58. Mongini F, Ciccone G, Rota E, Ferrero L, Ugolini A, Evangelista A, et al. Effectiveness of an educational and physical programme in reducing headache, neck and shoulder pain: a workplace controlled trial. Cephalalgia 2008;28: 541-52.
59. Fernandez-de-las-Penas C, Alonso-Blanco C, San-Roman J, Miangolarra-Page JC. Methodological quality of randomized controlled trials of spinal manipulation and mobilization in tension-type headache, migraine, and cervicogenic headache. J Orthop Sports Phys Ther 2006;36:160-9.
60. Lew HL, Lin PH, Fuh JL, Wang SJ, Clark DJ, Walker WC. Characteristics and treatment of headache after traumatic brain injury: a focused review. Am J Phys Med Rehabil 2006; 85:619-27.
[/et_pb_accordion_item][et_pb_accordion_item _builder_version=”3.0.106″ title=”Close Accordion” use_background_color_gradient=”off” background_color_gradient_start=”#2b87da” background_color_gradient_end=”#29c4a9″ background_color_gradient_type=”linear” background_color_gradient_direction=”180deg” background_color_gradient_direction_radial=”center” background_color_gradient_start_position=”0%” background_color_gradient_end_position=”100%” background_color_gradient_overlays_image=”off” parallax=”off” parallax_method=”on” background_size=”cover” background_position=”center” background_repeat=”no-repeat” background_blend=”normal” allow_player_pause=”off” background_video_pause_outside_viewport=”on” open_toggle_background_color=”#ffffff” closed_toggle_background_color=”#ffffff” text_shadow_style=”none” custom_padding=”0px|||” custom_padding_tablet=”0px|||” custom_padding_phone=”0px|||” box_shadow_style=”none” custom_css_main_element=”border:none;” custom_css_toggle_title=”font-size:0.8em;” custom_css_toggle_icon=”display:none;” /][/et_pb_accordion][/et_pb_column][/et_pb_row][/et_pb_section]
Post Disclaimer
Professional Scope of Practice *
The information herein on "Chiropractic Headache Treatment Guidelines in El Paso, TX" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Our information scope is limited to Chiropractic, musculoskeletal, physical medicines, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somatovisceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and/or functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.*
Our office has reasonably attempted to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez, DC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, RN*, CCST, IFMCP*, CIFM*, ATN*
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807, New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Florida
Florida License RN License # RN9617241 (Control No. 3558029)
License Compact Status: Multi-State License: Authorized to Practice in 40 States*
Presently Matriculated: ICHS: MSN* FNP (Family Nurse Practitioner Program)
Dr. Alex Jimenez DC, MSACP, RN* CIFM*, IFMCP*, ATN*, CCST
My Digital Business Card



