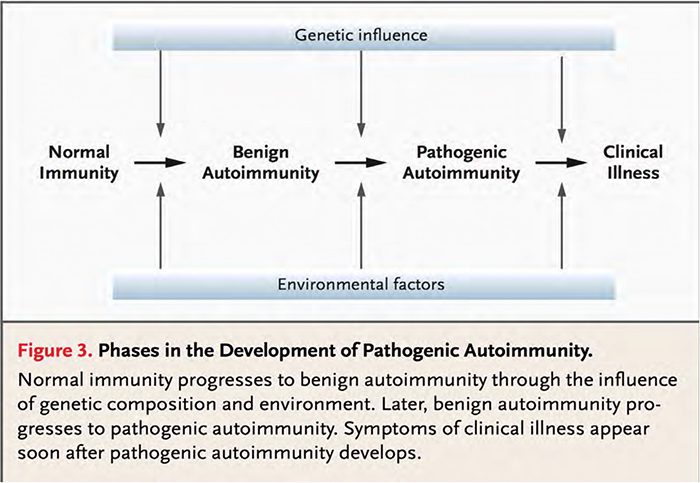
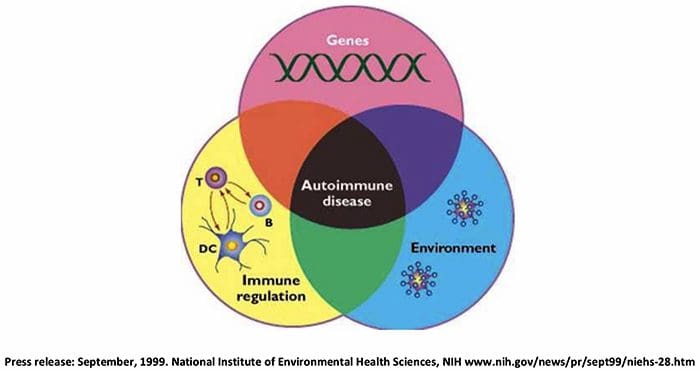
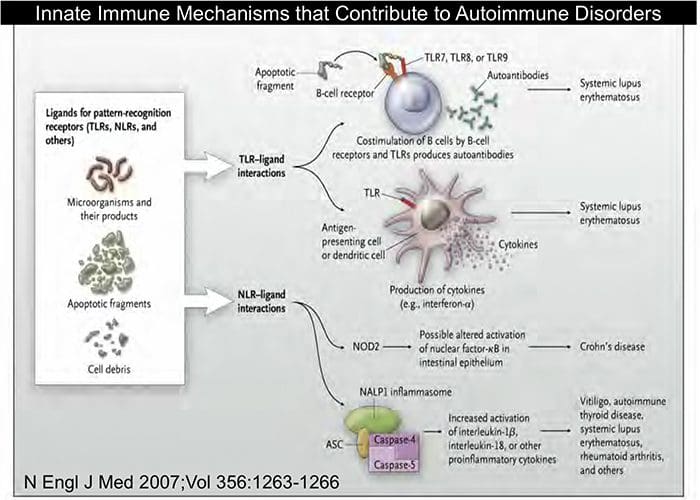
Autoimmunity is the reaction of cells (lymphocytes) or antibodies of the immune system along with the body’s own tissues leading to certain pathology. Autoimmunity can produce various conditions, which depend upon the target of the attack. While intrinsic factors, which include age, sex, and genetics contribute to autoimmunity, it is believed that extrinsic factors such as drugs, chemicals, microbes, and/or the environment can trigger the initiation of autoimmune responses.
Table of Contents
Autoimmune Disease & Environmental Toxicants
Educational Objectives
- Review air pollution, cigarette smoking, and citrullination as models for the genesis of autoimmune disease
- Explore the role of general cell stressors in autoimmune disease
- Discuss the impact of lung and gut barrier disruption by environmental toxins and food additives in autoimmune disease
- Utilize the Functional Medicine ATM model to illustrate the various mechanisms by which toxicants could contribute to the pathophysiology of autoimmune disease.
“Mild forms of the autoimmune response probably occur naturally in most people. But, for people with a predisposition to autoimmunity, environmental factors, such as toxic chemicals, drugs, bacteria or viruses, may trigger a full‐fledged response.”
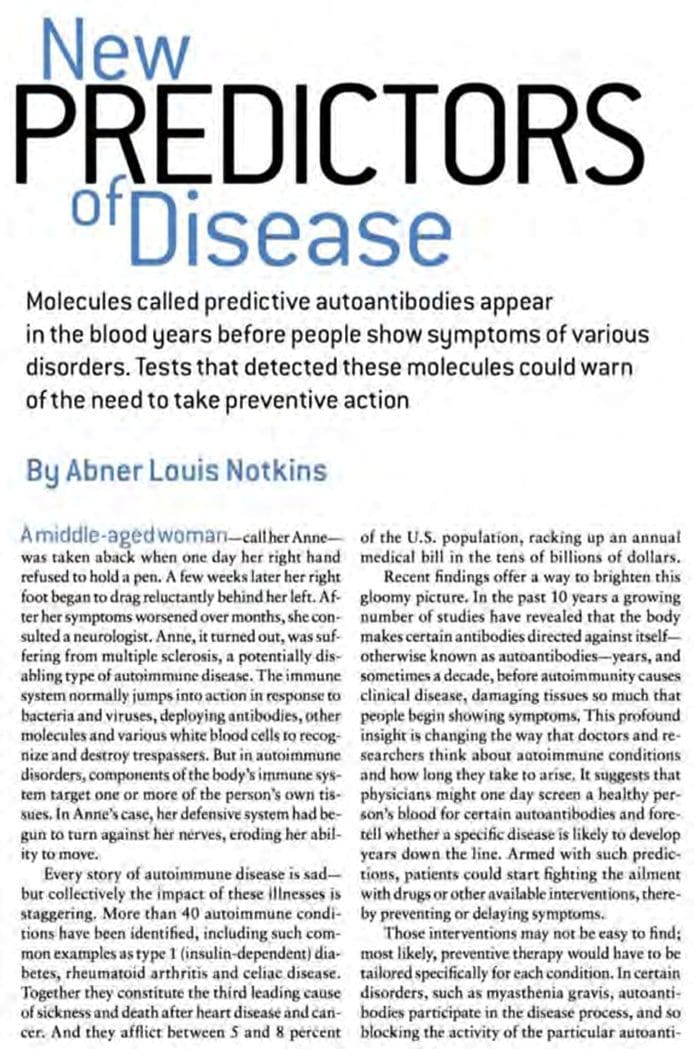
“NOVEL CRYSTAL BALL: One day Y‐shaped molecules called autoantibodies in a patient’s blood may tell doctors whether a patient is “brewing” certain diseases and may even indicate roughly how soon the individual will begin to feel symptoms.”
Autoimmune Disease: “Delayed Gratification”
Scientific American, March, 2007
- Many autoimmune diseases do not develop spontaneously, but instead evolve through an extended germination period before they become clinically evident…
- Well over 10 million people test positive for ANA, years before they have any symptoms.
- This implies the presence of additional environmental factors that dampen or amplify the process over time.
 Arbuckle MR, et al, N Engl J Med. 2003 Oct 16;349(16):1526‐33.
Arbuckle MR, et al, N Engl J Med. 2003 Oct 16;349(16):1526‐33.
Elevated Levels Of Antibodies Against Xenobiotics In A Subgroup Of Healthy Subjects
Vojdani, A, Kharrazian, D, Mukherjee, PS
- Some environmental chemicals, acting as haptens, can bind to a high‐ molecular‐weight carrier protein such as human serum albumin (HSA), causing the immune system to misidentify self‐tissue as an invader and launch an immune response against it, leading to autoimmunity
- The levels of specific antibodies against 12 different chemicals bound to HSA were measured by ELISA in serum from 400 blood donors.
- 10% (IgG) and 17% (IgM) of tested individuals showed significant antibody elevation against aflatoxin‐HSA adduct.
- The percentage of elevation against the other 11 chemicals ranged from 8% to 22% (IgG) and 13% to 18% (IgM).
- Detection of antibodies against various protein adducts may indicate chronic exposure to these chemical haptens in about 20% of the tested individuals
J Appl Toxicol. 2015 Apr; 35(4): 383–397.
Could Environmental Toxins Be A Key Missing Link That Pushes The Immune System Over The Brink To Permanently Lose Control Of Its Tolerance To Self‐Antigens?
(A Corollary Question: Does The Persistent Presence Of Autoantibodies Or Autoreactive T Cells Imply An Inevitable Progression To Full‐Blown Autoimmune Disease?)
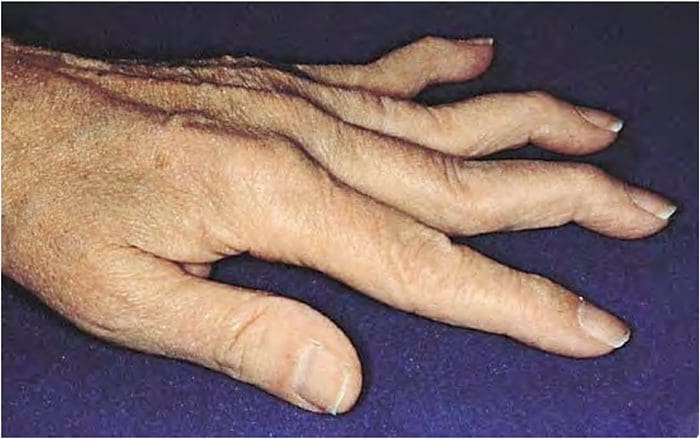
Rheumatoid Arthritis: Swan neck deformity from chronic synovitis
Anti‐Cyclic Citrullinated Peptide Antibody
- Current method is 96% specific for RA
- Elevated titers detected >10 years before onset of clinical disease
- Sensitivity (likelihood of positive test) increases from 50% at Dx to >75% over course of disease
- Likely involved in pathogenesis
- Citrullinated Ags are highly expressed in inflamed joints
- Positive test predicts joint erosion
- Antigen‐antibody complexes activate complement = inflammatory
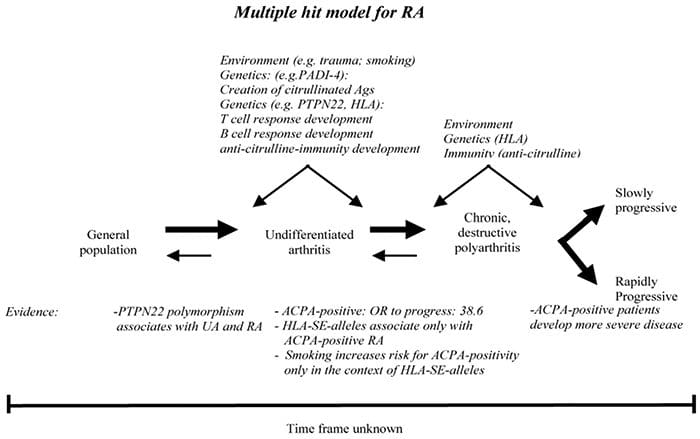
- Autoantibodies to citrullinated peptides
- Citrulline is formed by posttranslational modification of arginine residues by peptidyl arginine deiminases (PADs)
- PADs are upregulated by inflammation, injury, and toxicants
- Inflammation and injury thus increases citrullination of multiple synovial proteins
- Multiple HLA‐DR variants (shared epitope) associated with RA preferentially display citrullinated Ags on MHCII — activating citrulline‐specific autoreactive T cells
- Smoking increases risk of +anti‐CCP when coupled with HLR‐DR shared epitope
Floris van Gaalen et al. J Immunol 2005;175:5575-5580
Autoimmunity To Specific Citrullinated Proteins Gives The First Clues To The Etiology Of Rheumatoid Arthritis
Four citrullinated whole protein antigens, fibrinogen, vimentin, collagen type II, and alpha‐enolase, are now well established, with others awaiting further characterization
All four proteins are expressed in the joint, and there is evidence that antibodies to citrullinated fibrinogen and collagen type II mediate inflammation by the formation of immune complexes
Antibodies to citrullinated proteins are associated with HLA ‘shared epitope’ alleles
Porphyromonas gingivalis, pathogenic bacteria that is a major cause of periodontal disease, expresses endogenous citrullinated proteins
Thus, both smoking and Porphyromonas gingivalis are attractive etiological agents for further investigation into the gene/environment/autoimmunity triad of RA.
Wegner N, Lundberg K, Kinloch A, et al, Immunol Rev. 2010 Jan;233(1):34‐54
“More than 20,000 physicians, after Luckies had been furnished them for tests, basing their opinions on their smoking experience, stated that Luckies are less irritating than other cigarettes.”
Mad Men?
Holy Smokes!!
Cigarette Smoking Has Been Strongly Linked To Numerous Autoimmune Diseases
Cigarette Smoking & Autoimmune Disease: What Can We Learn From Epidemiology?
- Rheumatoid arthritis and cigarette smoking:
- Risk is highest in men: OR up to 4.4 X
- Smoking increases risk of seropositive RA 2.4X in women
- Smoking intensity and duration both greatly increase risk
- Smoking increases severity of symptoms
- Increased risk remains for 20 yrs after cessation
- “Cigarette smoking is the most conclusively established environmental risk factor for RA”
Costenbader, KH, Lupus, Vol. 15, No. 11, 737‐745 (2006)
Smoking & Air Pollution As Pro‐Inflammatory Triggers For The Development Of Rheumatoid Arthritis.
- Smoking initiates chronic inflammatory events in the lungs.
- These, in turn, promote the release of the enzymes, peptidylarginine deiminases 2 and 4 from smoke‐activated, resident and infiltrating pulmonary phagocytes.
- Peptidylarginine deiminases mediate conversion of various endogenous proteins to putative citrullinated autoantigens.
- In genetically susceptible individuals, these autoantigens trigger the production of autoantibodies to anti‐citrullinated peptide, an event which precedes the development of RA.
Anderson R, Meyer PW, Ally MM, Tikly M, Nicotine Tob Res. 2016 Jul;18(7):1556‐65
 Floris van Gaalen et al. J Immunol 2005;175:5575-5580
Floris van Gaalen et al. J Immunol 2005;175:5575-5580
Cigarette Smoking & Autoimmune Disease: What Can We Learn From Epidemiology?
- Systemic lupus erythematosis
- Highest risk in current smokers
- Current smokers have higher levels of anti‐dsDNA Ab
- Multiple sclerosis
- Increased risk of MS in both current & past smokers
- Risk increases with intensity of smoking (more cigarettes per day)
- Increased severity of MS in current smokers
- Cirtrullination of myelin‐basic protein ‐‐ antigenic
- Graves’ hyperthyroidism
- Smoking is esp. strong risk factor for opthalmopathy
- Primary biliary cirrhosis
- Smoking increases risk by 1.5 to 3x
Costenbader, KH, Lupus, Vol. 15, No. 11, 737‐745 (2006)
Industrial Air Emissions & Proximity To Major Industrial Emitters, Are Associated With Anti‐Citrullinated Protein Antibodies.
- Randomly sampled 1586 subjects out of 20,000 population from Quebec, Canada
- After adjusting for age, sex, smoking, and ethnicity, found
- Positive association between anti‐CCPA and annual industrial PM 2.5 and sulfur dioxide emissions (i.e. living closer to emitters increases anti‐CCPA)
- Negative association between anti‐CCPA and to a major industrial emitter of both PM 2.5 and SO2 (living further away from emitters decreases anti‐CCPA)
- “These analyses suggest that exposure to industrial emissions of air pollutants is related to ACCPA positivity.”
Bernatsky S, Smargiassi A, Joseph L, et al, Environ Res. 2017 Aug;157:60‐63
Air Pollution As A Determinant of Rheumatoid Arthritis
- The induction by air pollution of an inflammatory environment with high citrullination levels in the lung may induce iBALT formation, thereby causing a transition toward a more specific immune response via the production of anti‐citrullinated peptide antibodies.
- Air pollution not only triggers innate immune responses at the molecular level, increasing the levels of proinflammatory cytokines and reactive oxygen species, but is also involved in adaptive immune responses.
Thus, via the aryl hydrocarbon receptor (AHR), diesel exhaust particles can trigger a T‐cell switch to the Th17 profile.
Sigaux J, et al Joint Bone Spine. 2018 Mar 7. pii: S1297‐319X(18)30043‐5
The Aryl Hydrocarbon Receptor Links TH17‐Cell‐ Mediated Autoimmunity To Environmental Toxins
- The aryl hydrocarbon receptor (AhR) is a ligand‐dependent transcription factor that mediates a range of critical cellular events in response to halogenated aromatic hydrocarbons and non‐halogenated polycyclic aromatic hydrocarbons such as dioxin (TCDD)
- In a murine model of multiple sclerosis, which is mediated by Th17 cells, activation of cells using the AhR exacerbated disease, whereas mice deficient in the AhR had attenuated autoimmune disease.
- This paper thus links activation of Th17 cells with environmental toxins, suggesting a plausible hypothesis for the increase in such diseases with industrialization.
Veldhoen, M., Hirota, K., Westendorf, A.M, et al Nature. 2008 May 1;453(7191):106‐9
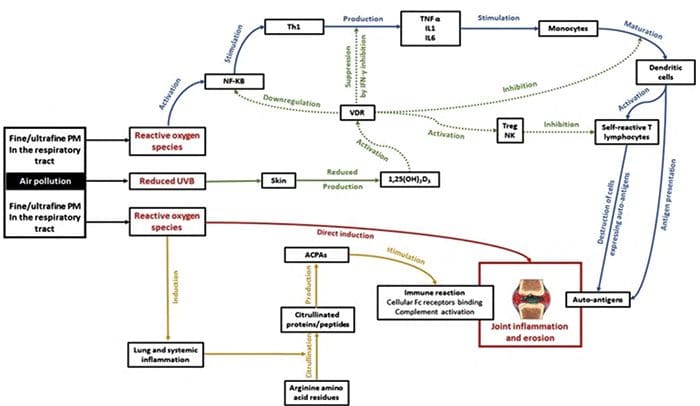 J Inflamm (Lond). 2015; 12: 48.
J Inflamm (Lond). 2015; 12: 48.
Does Rheumatoid Arthritis (& Other Autoimmune Diseases) Start In The Gut, Or In The Lungs?
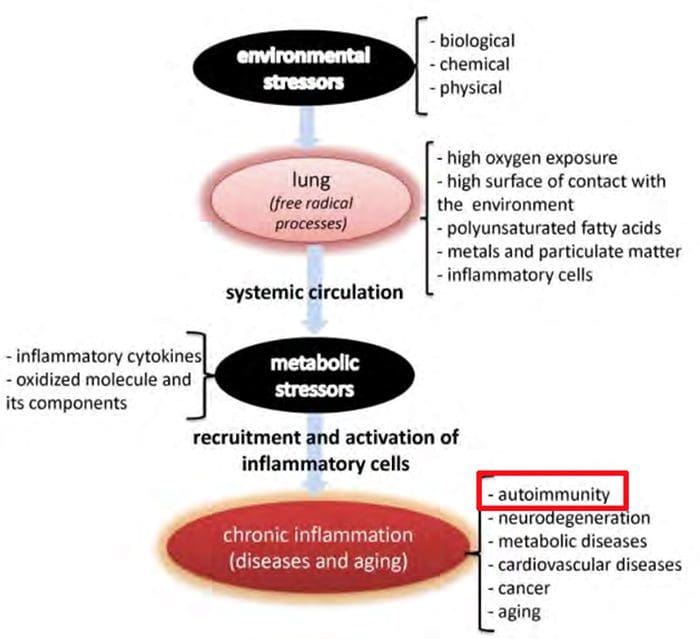 Gomez‐Mejiba SE, Zhai Z, Akram H, et al. Inhalation of Environmental Stressors & Chronic Inflammation: Autoimmunity and Neurodegeneration.
Gomez‐Mejiba SE, Zhai Z, Akram H, et al. Inhalation of Environmental Stressors & Chronic Inflammation: Autoimmunity and Neurodegeneration.
Mutation research. 2009;674(1‐2):62‐72.
Citrullination & Autoimmunity
- Environmental exposure to cigarette smoke and nanomaterials of air pollution may be able to induce citrullination in lung cells prior to any detectable onset of inflammatory responses, suggesting that protein citrullination could be considered as a sign of early cellular damage
- Citrullination has been reported to be a process present in a wide range of inflammatory tissues. Indeed, citrullinated proteins have been detected also in other inflammatory arthritides and in inflammatory conditions other than arthritides (multiple sclerosis, polymyositis, inflammatory bowel disease and chronic tonsillitis)
- Histone hypercitrullination can activate neutrophil extracellular traps (NETS)— high inflammatory
- These data support the hypothesis that rather than being a disease‐dependent process, citrullination is an inflammatory‐dependent condition that plays a central role in autoimmune diseases.
Valesini G, Shoenfeld Y, et al Autoimmun Rev. 2015 Jun;14(6):490‐7 Wang S,
Wang Y.Biochim Biophys Acta. 2013 Oct;1829(10):1126‐35
Air Pollution In Autoimmune Rheumatic Diseases: A Review
- Environmental factors contribute to the onset of autoimmune diseases, especially smoking and occupational exposure to silica dust in rheumatoid arthritis and systemic lupus erythematosus
- Scleroderma may be triggered by the inhalation of chemical solvents, herbicides and silica dust.
- Primary vasculitis associated with anti‐neutrophil cytoplasmic antibody (ANCA) may be triggered by silica exposure
- Air pollution is one of the environmental factors involved in systemic inflammation and autoimmunity
Farhat SC, et al, Autoimmun Rev. 2011 Nov;11(1):14‐21
Silica, Silicosis & Autoimmunity
- Exposure to respirable crystalline silica (<10 μm in size) occurs most often in occupational settings – the “dusty” trades
- Epidemiological studies link occupational exposure to crystalline silica dust with systemic lupus erythematosus, systemic sclerosis, and rheumatoid arthritis
- Findings from human and animal model studies are consistent with an autoimmune pathogenesis that begins with activation of the innate immune system leading to proinflammatory cytokine production (NLRP3 inflammasome), pulmonary inflammation leading to activation of adaptive immunity, breaking of tolerance, and autoantibodies and tissue damage
Pollard KM, Front Immunol. 2016; 7: 97.
Asbestos = Magnesium Silicate
Assessment Of Autoimmune Responses Associated With Asbestos Exposure In Libby, Montana, USA
- The population in Libby, Montana, provides a unique opportunity for study because of both occupational and environmental exposures that have occurred as a result of the mining of asbestos‐contaminated vermiculite near the community
- Libby serum samples showed significantly higher frequency of positive ANA and ENA tests, increased mean fluorescence intensity and titers of the ANAs, and higher serum IgA, compared with Missoula serum samples
- The results support the hypothesis that asbestos exposure is associated with autoimmune responses and suggests that a relationship exists between those responses and asbestos‐related disease processes.
Pfau JC, et al Environ Health Perspect, 2005, Vol 113: 25-30
Air Pollution, Oxidative Stress & Exacerbation Of Autoimmune Diseases
- Particulate matter present in air pollution can induce oxidative stress and cell death, both by apoptosis and necrosis of human cells leading to aggravation of chronic inflammation, i.e. the tissue damaging reaction observed in autoimmune diseases.
- Therefore, identification of strong inducers of oxidative stress among components of PM seems to be crucial for their neutralization and elimination from the ambient environment.
- It seems likely that PM 2.5 may exacerbate the onset of the SLE because they were attributed to a significant increase of the level of anti‐dsDNA antibodies, and the presence of the renal casts in SLE patients
- Exposure to ozone, sulphates, and other pollutants present in the air has been associated with type 1 diabetes in children
- MS occurrence and hospitalization was associated with exposure to air pollutants such as PM10, SO2, NO2, and NOx
- In addition to tobacco smoke and silica, pollution emissions from road traffic may be an environmental factor responsible for exacerbation of RA
Gawda, A, et al, Central European Journal of Immunology 2017; 42(3)
What Do Environmental Pollutants, Toxins, Infections & Unhealthy Diets Have In Common?
Environmental Toxicants, Oxidized PUFAs, Excessive Calories, Refined Sugars & AGEs…
- Increase inflammation and additional free radical production,
- Which damages tissues (bystander effect), disrupts barriers, and/or modifies DNA…
- Creating “foreign‐like” tissues that break immune tolerance (eg anti‐nuclear antibodies)
Cell Stressors
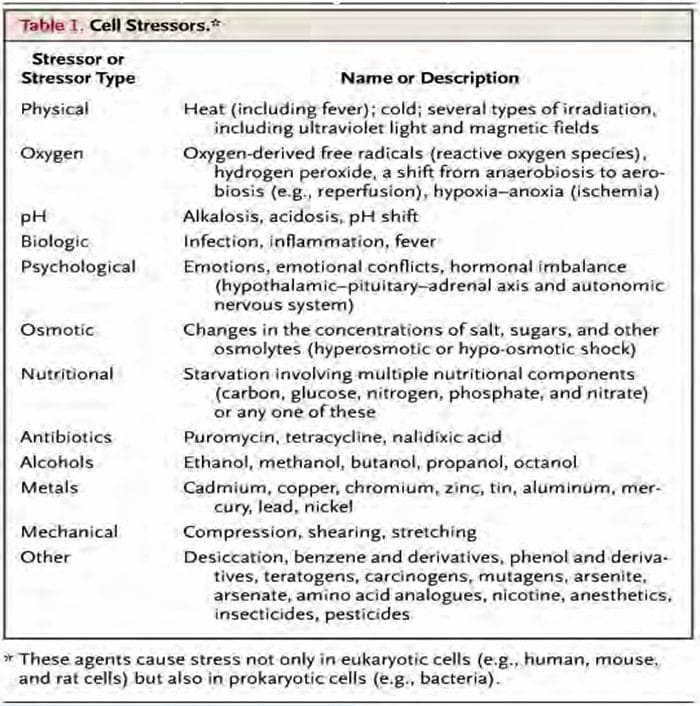 Macario, A. J.L. et al. N Engl J Med 2005;353:1489-1501
Macario, A. J.L. et al. N Engl J Med 2005;353:1489-1501
Damage Associated Molecular Patterns
- Molecular structures that activate immunologic receptors
- Released with cellular injury and/or necrosis after exposure to cellular stressors
- DNA fragments
- Mitochondria
- Misfolded proteins
- Advanced glycation end products have similar biological effects
- Initiate and perpetuate inflammatory response (esp NLRP3 inflammasome)
Ojcius D, Saïd‐Sadier N. Alarmins, inflammasomes and immunity. Biomedical Journal. 2012;35(6):437.
Vakrakou AG, Boiu S, Ziakas PD, et al, Systemic activation of NLRP3 inflammasome in patients with severe primary Sjögren’s syndrome fueled by inflammagenic DNA accumulations.
J Autoimmun. 2018 Mar 15. pii: S0896‐8411(17)30789‐8.
Environmental Xenobiotic Exposure & Autoimmunity
- We argue that localized tissue damage and chronic inflammation elicited by xenobiotic exposure leads to the release of self‐antigens and damage‐associated molecular patterns …
- As well as the appearance of ectopic lymphoid structures and secondary lymphoid hypertrophy,
- Which provide a milieu for the production of auto-reactive B and T cells that contribute to the development and persistence of autoimmunity in predisposed individuals.
Pollard KM, Christy JM, Cauvi DM, Kono DH, Current Opinion in Toxicology, Volume 10, August 2018, Pages 15‐22
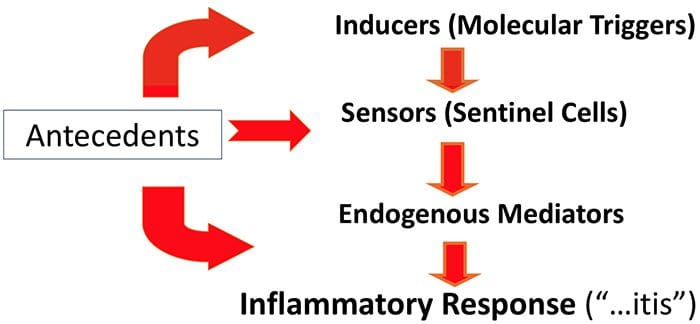
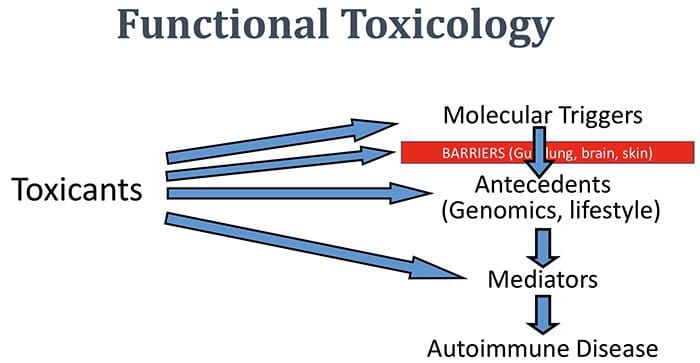
The Functional Medicine Paradigm (Slightly Modified)
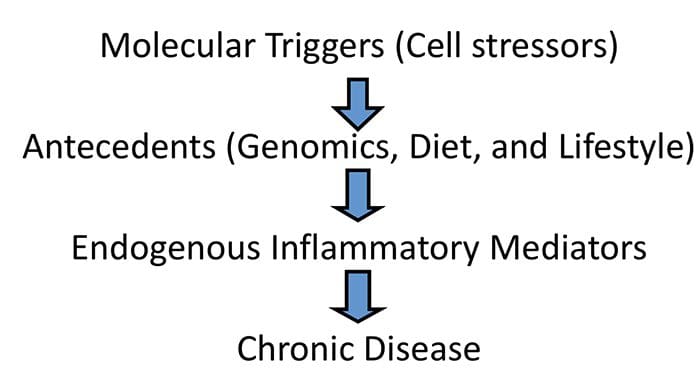
The Inflammatory Process: A Physiologic Algorithm
Toxicants & Autoimmunity: General Mechanisms
-
Effect on antecedents:
- Genetic/epigenetic alterations: eg altered methylation, acetylation
- Damaged membrane barriers (leaky gut, skin, brain) allowing increased exposure to triggers
- Immune disruption = increased susceptibility to triggers
- Overload in hepatic detoxification pathways
-
Effect on triggers:
- Synergistic action (immunotoxicant)
- Adjuvant: chemical modification of self‐antigen to make it appear foreign or immunogenic (neoantigens)
- Enhanced apoptosis: danger/damage signals (DAMPs)
-
Effect on mediators:
- Amplified inflammatory pathways
- Increased oxidative stress
- Disruption of pro‐resolution counter‐regulatory mechanisms
Functional Toxicology


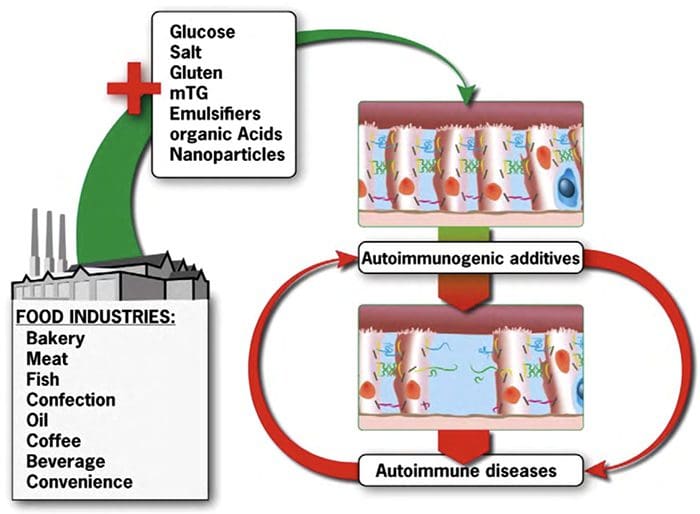
Changes In Intestinal Tight Junction Permeability Associated With Industrial Food Additives Explain The Rising Incidence Of Autoimmune Disease
- The incidence of autoimmune diseases and food additive consumption are both increasing in parallel
- Dysfunction of intestinal tight junctions is common in multiple autoimmune diseases
- Commonly used industrial food additives including glucose, salt, solvents, emulsifiers, gluten, microbial transglutaminase, and nanoparticles increase intestinal tight junction leakage.
- Intestinal entry of foreign antigen activates the autoimmune cascade
Lerner A, Matthias T. Autoimmunity Reviews 14 (2015) 479–489
 Autoimmunity Reviews 14 (2015) 479–489
Autoimmunity Reviews 14 (2015) 479–489
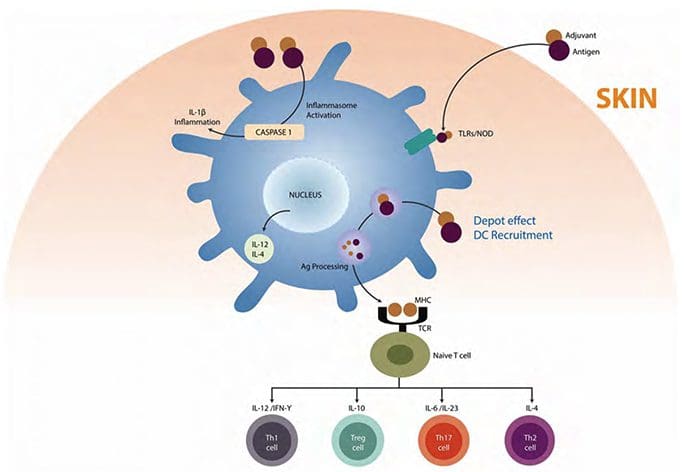
Autoimmune Disease: “Two‐Hit” Signal Theory
- Barrier disruption allows immune system to be repeatedly exposed to a combination of an autoantigen & an “adjuvant” [Adjuvants can be toxicants, microbes, foods]
- This triggers a genetically predisposed immune system to react to the autoantigen as a non‐self “stranger”
- “Danger” signals released at the site of clearance of dead cells amplify the process; shaping the features & severity of the resulting autoimmune disease
- Persistent “Stranger + Danger” = loss of tolerance
- Based on this model, strategies aimed at preventing the accumulation of dying cells lowering the adjuvant (toxic) load may be beneficial for the prevention & treatment of autoimmune disease
 Anaya JM, Ramirez‐Santana C, Alzate MA, Molano‐Gonzalez N, Rojas‐Villarraga A, The Autoimmune Ecology., Front Immunol. 2016 Apr 26;7:139
Anaya JM, Ramirez‐Santana C, Alzate MA, Molano‐Gonzalez N, Rojas‐Villarraga A, The Autoimmune Ecology., Front Immunol. 2016 Apr 26;7:139
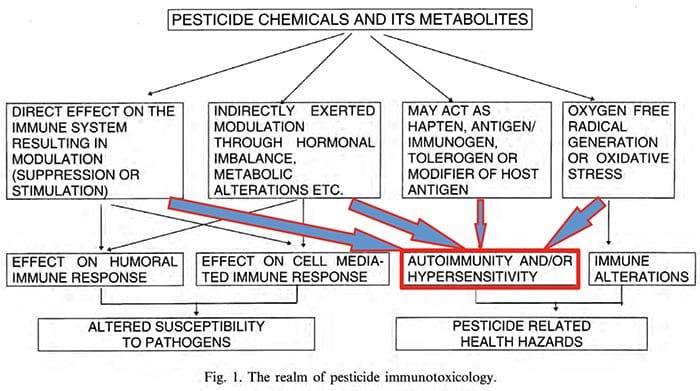 Bannerjee, B.D., Toxicology Letters, 1999, Vol 107: 21-31
Bannerjee, B.D., Toxicology Letters, 1999, Vol 107: 21-31
Oxidatively Modified Autoantigens In Autoimmune Diseases
- Oxidative modification of proteins has been shown to elicit antibodies in a variety of diseases, including SLE, diabetes mellitus & RA.
- Oxidatively modified DNA & LDL occur in SLE, a disease in which premature atherosclerosis is a serious problem. AGE pentosidine & AGE‐modified IgG have been shown to correlate with RA disease activity.
- In the face of overwhelming evidence for the involvement of oxidative damage in autoimmunity, the administration of antioxidants is a viable untried alternative for preventing or ameliorating autoimmune disease…”
Kurien BT, Hensley K, Bachmann M, Scofield RH., Free Rad Biol & Med, 2006, Vol 41: 549-556
Oxidative Stress In The Pathology & Treatment Of Systemic Lupus Erythematosus.
- Oxidative stress is increased in SLE, and it contributes to immune system dysregulation, abnormal activation and processing of cell‐ death signals, autoantibody production and fatal comorbidities.
- Oxidative modification of self antigens triggers autoimmunity, and the degree of such modification of serum proteins shows striking correlation with disease activity and organ damage in SLE.
- Reactive oxygen intermediates (ROI) mostly originate from mitochondria, and T cells from patients with SLE exhibit mitochondrial dysfunction
- In T cells from patients with SLE and animal models of the disease, glutathione, the main intracellular antioxidant, is depleted and serine/threonine‐protein kinase mTOR undergoes redox‐dependent activation.
- In turn, reversal of glutathione depletion by application of its amino acid precursor, N‐acetylcysteine, improves disease activity in lupus‐ prone mice; pilot studies in patients with SLE have yielded positive results that warrant further research.
- Antioxidant therapy might also be useful in ameliorating damage caused by other treatments.
Perl, A, Nat Rev Rheumatol. 2013 Nov;9(11):674‐86
Environmental Agents, Oxidative Stress & Autoimmunity
- Oxidative stress (OS) plays an important role in the pathogenesis of a variety of autoimmune diseases (ADs) and many environmental agents participate in this process.
- Environmental agents, including trichloroethylene (TCE), silica, pristane (TMPD in mineral oil), mercury, and smoke, are known to induce an autoimmune response, potentially through OS‐mediated mechanisms.
- Antioxidants can attenuate SLE disease activity by down regulating NLRP3 inflammasome activation and activating Nrf2 signaling.
Khan MF, Wang G. Curr Opin Toxicol. 2018 Feb;7:22‐27.
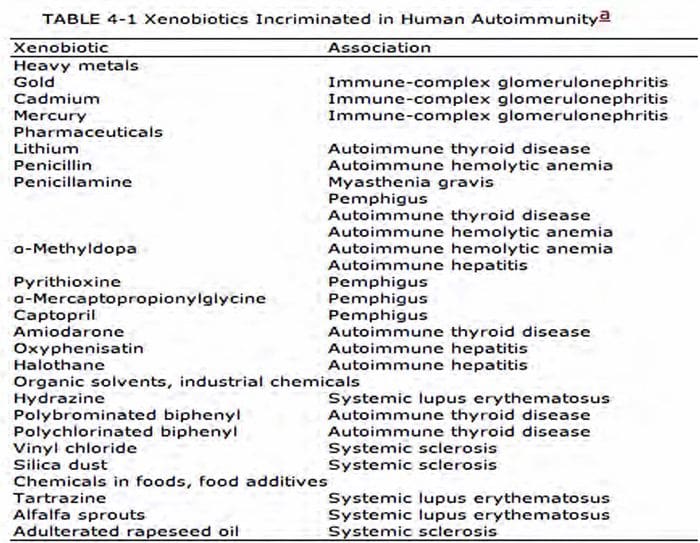
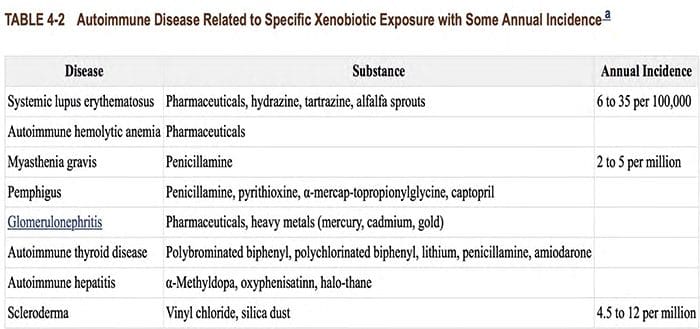
Xenobiotics Associated With Autoimmune Diseases
- Organochlorines (dioxin, PCBs) & polyvinyl chloride
- Polybrominated biphenyls
- Organic solvents: benzene, toluene, trichloroethylene
- Polycyclic aromatic hydrocarbons (cigarette smoke, automotive exhaust, charbroiled meat)
- Hydrazines: rocket fuels
- Airborne particulates
- Pharmaceuticals & inhalant anesthetics
- Preservatives (formaldehyde)
- Permanent hair dyes
- Food dyes (tartrazine)
- L‐canavanine (in alfalfa sprouts), an arginine analog
- Adulterated rapeseed oil (aniline‐denatured):“Spanish toxic oil syndrome”
- L‐tryptophan (contaminated): eosinophilic myositis
Metals & Minerals Associated With Autoimmune Diseases
-
Heavy metals
- Mercury
- Cadmium
- Lead
- Gold
-
Minerals & Metalloids
- Silica (crystalline silicon dioxide)
- Asbestos (chrysotile = magnesium silicate)
- Arsenic
- Lithium
- Iodine
Bigazzi PE., Metals and kidney autoimmunity. Environ Health Perspect. 1999 Oct;107 Suppl 5:753‐65
Biologic Markers in Immunotoxicology National Research Council (US) Subcommittee on Immunotoxicology. Washington (DC): National Academies Press (US); 1992.
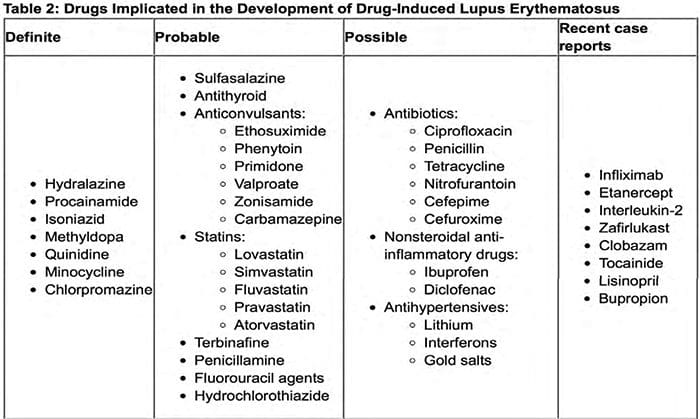 Garza, A, Drug‐Induced Autoimmune Diseases. Pharmacy Times 1‐20‐16
Garza, A, Drug‐Induced Autoimmune Diseases. Pharmacy Times 1‐20‐16
http://www.pharmacytimes.com/publications/issue/2016/january2016/drug‐induced‐autoimmune‐diseases
“Lupus Erythematosus & Other Autoimmune Diseases Related To Statin Therapy: A Systematic Review”
- 28 published cases of statin‐induced autoimmune disease:
- 10 cases SLE (2 with autoimmune hepatitis)
- 3 cases subacute cutaneous SLE
- 14 cases dermatomyositis & polymyositis
- Most cases needed systemic immunosuppression
- In many patients, antinuclear antibodies were still positive many months after clinical recovery
Noel, B; J Eur Acad Dermatol Venereol 2007; 21(1):17‐24
Putting It All Together…
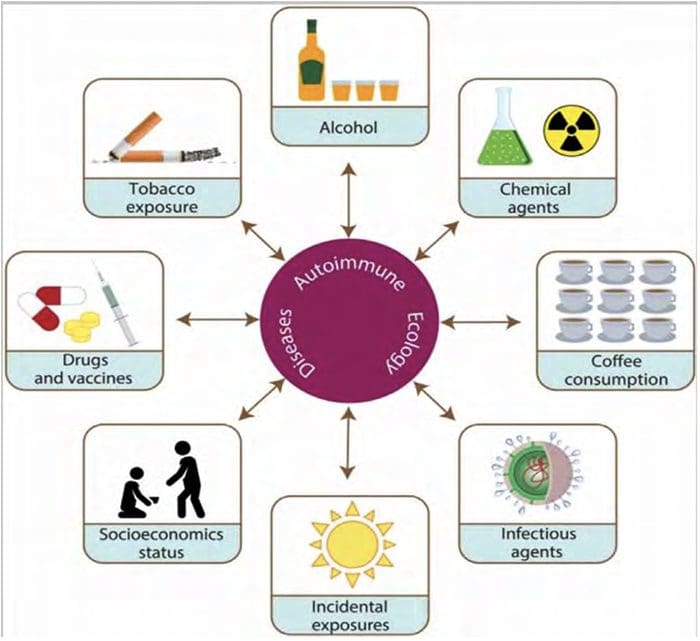 Anaya JM, et al, The Autoimmune Ecology., Front Immunol. 2016 Apr 26;7:139
Anaya JM, et al, The Autoimmune Ecology., Front Immunol. 2016 Apr 26;7:139
Messages To Take Home
- Autoimmune and autoinflammatory diseases are steadily increasing in our society
- The rise in exposure to environmental pollutants and other toxins is increasing the total body burden of xenobiotics
- A central theme in the development of autoimmune diseases is the loss of immune tolerance
- Immune tolerance can be broken by disruption of barriers (skin, lung, gut, brain) and/or immune dysregulation
- Numerous xenobiotics have been shown to disrupt healthy barriers and dysregulate immune responses
- Xenobiotics may play a central role in the initiation and perpetuation of autoimmune disease
Explosion Of Autoimmune Diseases: The Mosaic Of Old & Novel Factors
- Modern life and exposures to novel chemical and xenobiotic compounds may lead to the development of new complexes of symptoms that do not necessarily belong to one of the well‐known autoimmune diseases
- As physicians and scientists, we must continue to study novel pathogenic mechanisms and susceptible alleles to help us identify new therapeutic venues.
Agmon‐Levin N, Lian Z, Shoenfeld Y. Cell Mol Immunol. 2011 May; 8(3): 189–192.
 IFM Annual International Conference Hollywood, Florida May, 2018
IFM Annual International Conference Hollywood, Florida May, 2018
Robert Rountree, MD
Robert Rountree, MD is a speaker, consultant, and advisory board member for Thorne and Balchem. He is also a clinical trial board member for Thorne Research.
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card







Comments are closed.