Table of Contents
Introduction
The brain’s main function in the central nervous system is to send out neuron signals all throughout the body. What this does is that these signals go from the brain through the spinal cord and send out the information for the body to function and vice versa. These signals make sure that the organ system is doing its job properly and making the body move as well. When there are unwanted pathogens entering the body, it can disrupt the neuron signals from reaching the brain and cause chronic symptoms that can develop over time causing the person pain. In this 2 part series, we will be taking a look at how cortisol and inflammation affect the brain as well as how the gut and the brain make a connection. Part 1 discussed what is the central nervous system and what factors can affect the brain. By referring patients to qualified and skilled providers who specialized in neurological services. To that end, and when appropriate, we advise our patients to refer to our associated medical providers based on their examination. We find that education is the key to asking valuable questions to our providers. Dr. Alex Jimenez DC provides this information as an educational service only. Disclaimer
Can my insurance cover it? Yes, in case you are uncertain here is the link to all the insurance providers we cover. If you have any questions, please call Dr. Jimenez at 915-850-0900.
The Central Nervous System
The central nervous system is consist of the brain and the spinal cord in the body. What this system does, as research shows, is that it signals all the neurons in the body and transports them back and from the brain to the entire body. Each nerve signal makes sure that the entire body is moving and each organ system is getting the signals and sending them back to the brain. Some of the functions that the central nervous system does are that it controls how a person breathes, releases hormones, controls body temperature, and controls emotions as studies show. With the brain’s main function is to send out signals throughout the body, surprisingly, some of the factors can actually affect the brain signal if it becomes too chronic and they are cortisol and inflammation.
Cortisol & The Brain
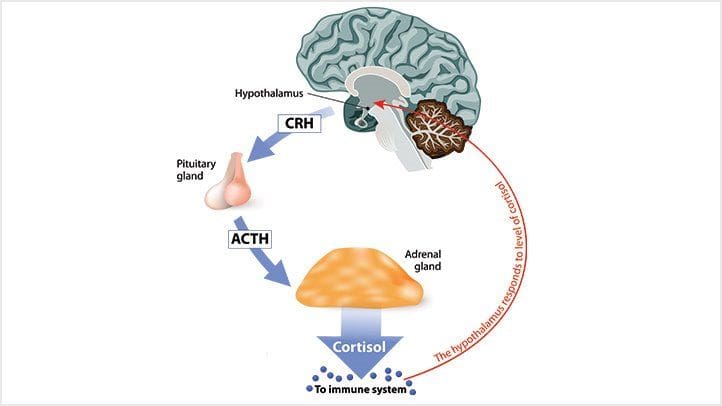
Now cortisol is a stress hormone that gives the body a little boost of energy when an individual is dealing with a situation. Even though stress can be beneficial to the body it can also become chronic if it is not taken care of. Too much stress can lead to chronic pain and as studies have found, cortisol is released by the activation of the HPA (hypothalamic-pituitary-adrenal) axis, and when that increases can lead to age-related cognitive disorders in the brain. Other studies have found that when there is long-term elevated cortisol affecting the brain it can negatively influence cardiometabolic changes in the body. See the brain can send signals to the endocrine system to release hormones to get the body to function at normal levels, but when cortisol levels begin to rise in the body it can affect the brain.
Other studies have shown that when stress begins in the brain and starts to affect it, can cause pathophysiology changes to the neural, cardiovascular, immune, and metabolic systems in the body. The brain gives the signal of a “fight or flight” response to the body as it endures stressful situations. When the cortisol levels become chronic, the brain signals will be disruptive and cause chronic symptoms to develop over time and cause the individual pain.
Inflammation & The Brain
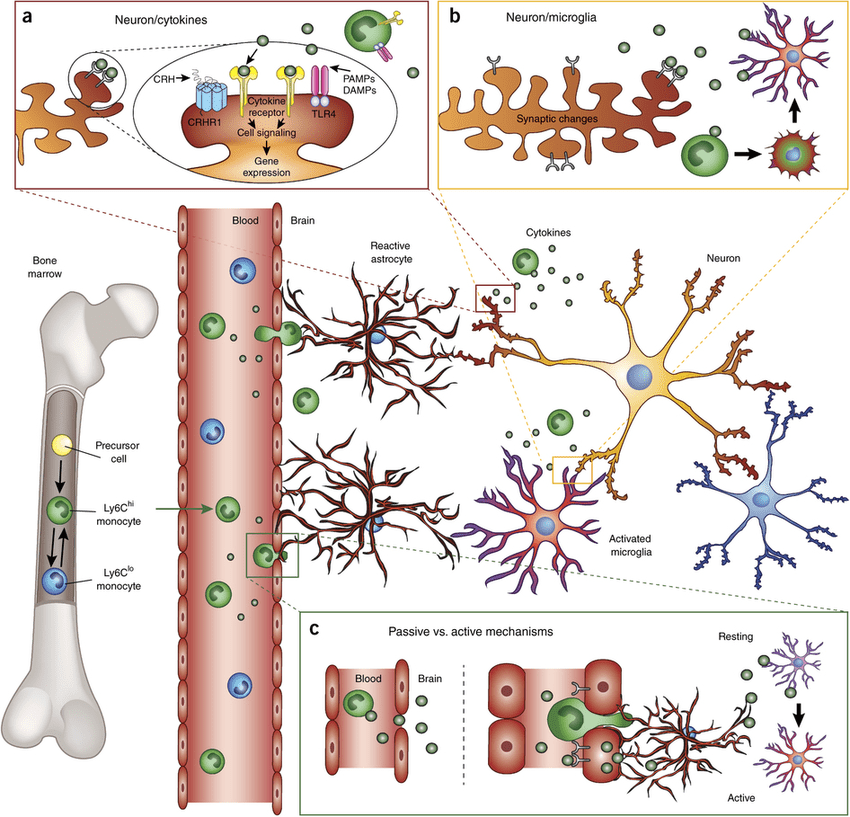
Just like cortisol, inflammation does the same thing to the body. When there are unwanted pathogens entering the body and causing havoc, the immune systems send out inflammatory cells to the affected area and attack the pathogen. Studies have found that inflammatory cytokines are produced by the nervous system to produce behavioral symptoms and characteristics of the illness to stop the infection from spreading and healing the body.
However, if the inflammatory cells start to attack the body out of nowhere and there are no unwanted pathogens attacking the body, then it can become chronic. Studies have found that chronic inflammation can increase the peptides and age can become the risk factor for Alzheimer’s disease while also becoming a role in the development of neurodegeneration.
HCTP Therapy
HCTP (human cellular tissue products) or stem cells* have been used in regenerative therapy treatments in both international and nationally affiliated clinics and distribution organizations to help individuals with chronic pain. HCTP has been used to help boost up the body’s own natural healing process by regenerating and repairing damaged tissues, diseased organs, and cellular structure back to their original state in the body. With more upcoming research discussing about the beneficial properties of HCTP, it can help the individual be pain-free and let them continue their wellness journey.
The Gut-Brain Connection
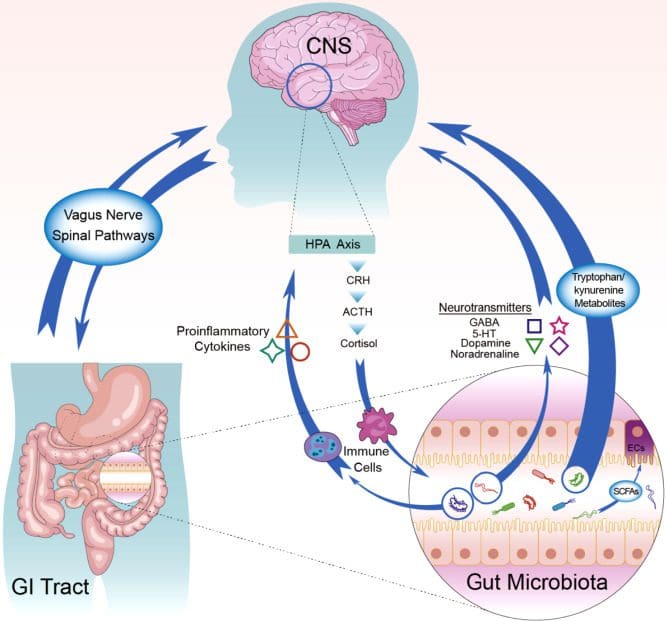
Research studies have found that the gut and brain are connected to each other as they send a bidirectional connection to each other and promote the proper maintenance of gastrointestinal homeostasis. Other articles have talked about how the brain and gut are even more connected through the endocrine system. While the effects from the gut microbiota can help regulate the neurotransmitters from the brain and the brain’s effects on the gut can help intestinal development and barrier integrity and function as studies show. When unwanted pathogens like chronic inflammation and chronic cortisol affect both the gut and the brain, it can cause the body to be dysfunctional and can cause the individual person pain in their body.
Conclusion
All in all, by regulating cortisol and inflammation levels in the body can provide beneficial results to the brain signals to be functioning normally. By eating nutritious food, making small changes in a certain lifestyle, and exercising regularly can help the individual get their life together and be pain-free. Not only that but keeping a healthy brain can dampen the effects of neurodegenerative disorders from progressing even further as the body ages naturally and the brain is “young” and healthy.
Reference
Blasko, Imrich, et al. “How Chronic Inflammation Can Affect the Brain and Support the Development of Alzheimer’s Disease in Old Age: The Role of Microglia and Astrocytes.” Aging Cell, U.S. National Library of Medicine, Aug. 2004, https://pubmed.ncbi.nlm.nih.gov/15268750/.
Braniste, Viorica, et al. “The Gut Microbiota Influences Blood-Brain Barrier Permeability in Mice.” Science Translational Medicine, U.S. National Library of Medicine, 19 Nov. 2014, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4396848/.
Carabotti, Marilia, et al. “The Gut-Brain Axis: Interactions between Enteric Microbiota, Central and Enteric Nervous Systems.” Annals of Gastroenterology, Hellenic Society of Gastroenterology, 2015, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4367209.
de Souza-Talarico, Juliana Nery, et al. “Effects of Stress Hormones on the Brain and Cognition: Evidence from Normal to Pathological Aging.” Dementia & Neuropsychologia, Associação De Neurologia Cognitiva e Do Comportamento, 2011, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5619133/.
Echouffo-Tcheugui, Justin B, et al. “Circulating Cortisol and Cognitive and Structural Brain Measures: The Framingham Heart Study.” Neurology, Lippincott Williams & Wilkins, 20 Nov. 2018, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6260201/.
Ludwig, Parker E. “Neuroanatomy, Central Nervous System (CNS).” StatPearls [Internet]., U.S. National Library of Medicine, 14 Oct. 2021, https://www.ncbi.nlm.nih.gov/books/NBK442010/.
McEwen, Bruce S. “Central Effects of Stress Hormones in Health and Disease: Understanding the Protective and Damaging Effects of Stress and Stress Mediators.” European Journal of Pharmacology, U.S. National Library of Medicine, 7 Apr. 2008, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2474765/.
Newman, Tim. “Central Nervous System: Structure, Function, and Diseases.” Medical News Today, MediLexicon International, 3 Feb. 2022, https://www.medicalnewstoday.com/articles/307076.
Sartori, Andrea C, et al. “The Impact of Inflammation on Cognitive Function in Older Adults: Implications for Healthcare Practice and Research.” The Journal of Neuroscience Nursing: Journal of the American Association of Neuroscience Nurses, U.S. National Library of Medicine, Aug. 2012, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3390758/.
Disclaimer
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card



Comments are closed.