Can working individuals dealing with degenerative pain syndrome incorporate decompression to provide body relief and mobility?
Table of Contents
Introduction
As part of the musculoskeletal system, the spine allows the body to stand vertically and helps protect the spinal cord from injuries. Since the central nervous system provides neuron signals from the brain to the nerve roots, the human body can be mobile without pain or discomfort. This is due to the spinal discs between the facet joints, which can be compressed, absorb the vertical axial pressure, and help distribute the weight to the lower and upper extremity muscles. However, as many people realize, repetitive movements and wear and tear on the spinal structure can lead to overlapping risk profiles that can cause the spinal disc to degenerate and invoke pain in the musculoskeletal system. To that point, it can cause the individual to be in extreme pain and discomfort over time. Today’s article looks at how degenerative pain syndrome affects the spine, the symptoms it’s associated with, and how decompression can reduce degenerative pain syndrome. We talk with certified medical providers who consolidate our patients’ information to provide numerous treatments to relieve degenerative pain syndrome that is causing mobility issues on the spine. We also inform and guide patients on how decompression can help reduce the pain-like symptoms correlating with degenerative pain syndrome. We encourage our patients to ask their associated medical providers intricated and important questions about the referred pain-like symptoms they are experiencing from degenerative pain that is affecting their quality of life. Dr. Jimenez, D.C., incorporates this information as an academic service. Disclaimer.
Degenerative Pain Syndrome On The Spine
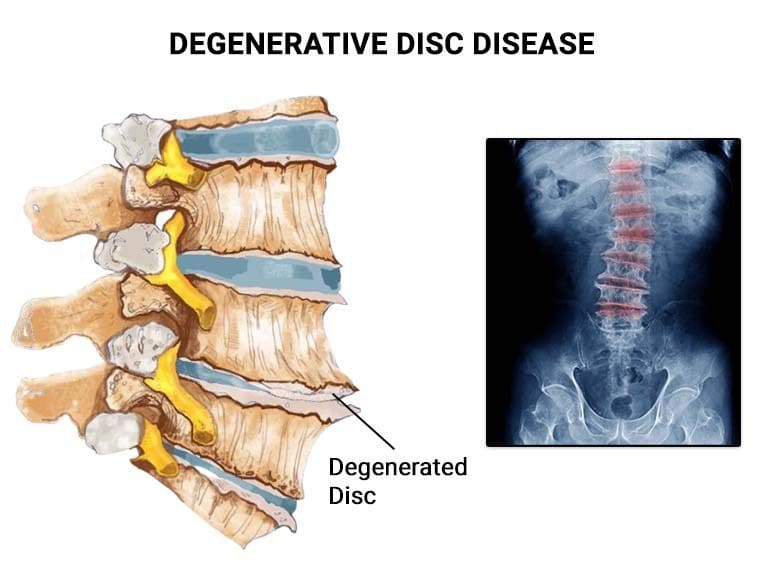
Do you feel muscle aches or pains in your back after an extended period of lying down, sitting, or standing? Do you feel constant pain after carrying a heavy object from one location to another? Or does twisting or turning your torso provide temporary relief? Many people often don’t realize that many of these pain-like issues are associated with degenerative pain syndrome that affects the spine. Since the body ages naturally, the spine does as well through degeneration. When the spinal discs start to degenerate, it can cause the vertical axial pressure to flatten and squeeze the disc, disrupting its ability to keep hydrated and causing it to protrude out of its original position. At the same time, the height of the spinal disc will gradually fall, and the consequence is a change in dynamics in the affected spine segments. (Kos et al., 2019) Degeneration can cascade down to the surrounding ligaments, muscles, and joints when degeneration starts to affect the spine.
The Symptoms Associated With Degenerative Pain
When the surrounding joints, muscles, and ligaments are affected by degenerative disc pain, it can be due to multiple factors contributing to the pain-like symptoms. Inflammation is one of the symptoms that are associated with degenerative pain syndrome, as disturbances can affect the circadian rhythm and disrupt homeostasis, which then leads to increased stress on the spinal disc, which then contributes to the degenerative process. (Chao-Yang et al., 2021) Inflammation can cause the affected muscles to be inflamed and cause more overlapping risk profiles, as it can affect the upper and lower extremities. Additionally, mechanical loading may affect disc degeneration in various ways at the different vertebral levels. (Salo et al., 2022) This can lead to pain-like symptoms like:
- Arm and leg tenderness
- Nerve pain
- Loss of sensory functions on the upper and lower extremities
- Tingling sensations
- Muscle pain
However, numerous treatments can help restore spinal mobility and lessen the painful effects of the degenerative pain syndrome of the spine.
The Non-Surgical Approach To Wellness- Video
When it comes to seeking treatment for degenerative pain syndrome, many individuals will do research on which treatment is affordable for their pain, hence why many people opt for non-surgical treatment to alleviate their pain. Non-surgical treatments are customized to the individual’s pain. They can help kickstart the person’s wellness journey, which can include a combination of exercise, manual therapy, and lifestyle modifications. (Brogger et al., 2018) The video above shows how a non-surgical approach can benefit someone with degenerative pain syndrome affecting their spine.
Decompression Reducing Degenerative Pain Syndrome

With many available treatments to reduce pain-like symptoms affecting the spine, non-surgical treatments can be an option. Ranging from chiropractic care to acupuncture, non-surgical treatments can be combined to minimize the pain-like effects. Decompression, as part of the non-surgical treatment options, is an excellent way to reduce the degenerative pain process in the spine. Decompression allows the spinal column to be gently pulled through a traction machine to relieve the spinal disc. When a traction machine decomposes the spine, the pain intensity is significantly reduced in all body parts. (Ljunggren et al., 1984) This is due to negative pressure being reinstated back to the spine to increase disc height and restore the nutrients back to the affected disc and rehydrate them. (Choi et al., 2022) When people start incorporating decompression through consecutive treatment, their pain intensity is reduced, and their spine is mobile again while slowing down the degenerative process on the spine. This allows them to take better care of their bodies by making small changes in their health and wellness.
References
Brogger, H. A., Maribo, T., Christensen, R., & Schiottz-Christensen, B. (2018). Comparative effectiveness and prognostic factors for outcome of surgical and non-surgical management of lumbar spinal stenosis in an elderly population: protocol for an observational study. BMJ Open, 8(12), e024949. https://doi.org/10.1136/bmjopen-2018-024949
Chao-Yang, G., Peng, C., & Hai-Hong, Z. (2021). Roles of NLRP3 inflammasome in intervertebral disc degeneration. Osteoarthritis Cartilage, 29(6), 793-801. https://doi.org/10.1016/j.joca.2021.02.204
Choi, E., Gil, H. Y., Ju, J., Han, W. K., Nahm, F. S., & Lee, P.-B. (2022). Effect of Nonsurgical Spinal Decompression on Intensity of Pain and Herniated Disc Volume in Subacute Lumbar Herniated Disc. International Journal of Clinical Practice, 2022, 1-9. https://doi.org/10.1155/2022/6343837
Kos, N., Gradisnik, L., & Velnar, T. (2019). A Brief Review of the Degenerative Intervertebral Disc Disease. Med Arch, 73(6), 421-424. https://doi.org/10.5455/medarh.2019.73.421-424
Ljunggren, A. E., Weber, H., & Larsen, S. (1984). Autotraction versus manual traction in patients with prolapsed lumbar intervertebral discs. Scand J Rehabil Med, 16(3), 117-124. https://www.ncbi.nlm.nih.gov/pubmed/6494835
Salo, S., Hurri, H., Rikkonen, T., Sund, R., Kroger, H., & Sirola, J. (2022). Association between severe lumbar disc degeneration and self-reported occupational physical loading. J Occup Health, 64(1), e12316. https://doi.org/10.1002/1348-9585.12316
Disclaimer
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card



Comments are closed.