Stiffness and Pain Developing In The Shoulder
Stiffness and pain developing in the shoulder could be adhesive capsulitis, (frozen shoulder), a condition in the shoulder’s ball-and-socket joint/glenohumeral joint. It usually develops over time and limits the functional use of the arm. The pain and tightness restrict arm movement, and the duration of symptoms can persist for 12-18 months. The cause is often unknown, but it is more common in individuals over 40, individuals with diabetes, thyroid disease, and cardiac conditions have an increased risk of developing the condition, and women tend to develop the condition more than men. Chiropractic treatment can be effective at relieving pain and expediting recovery.
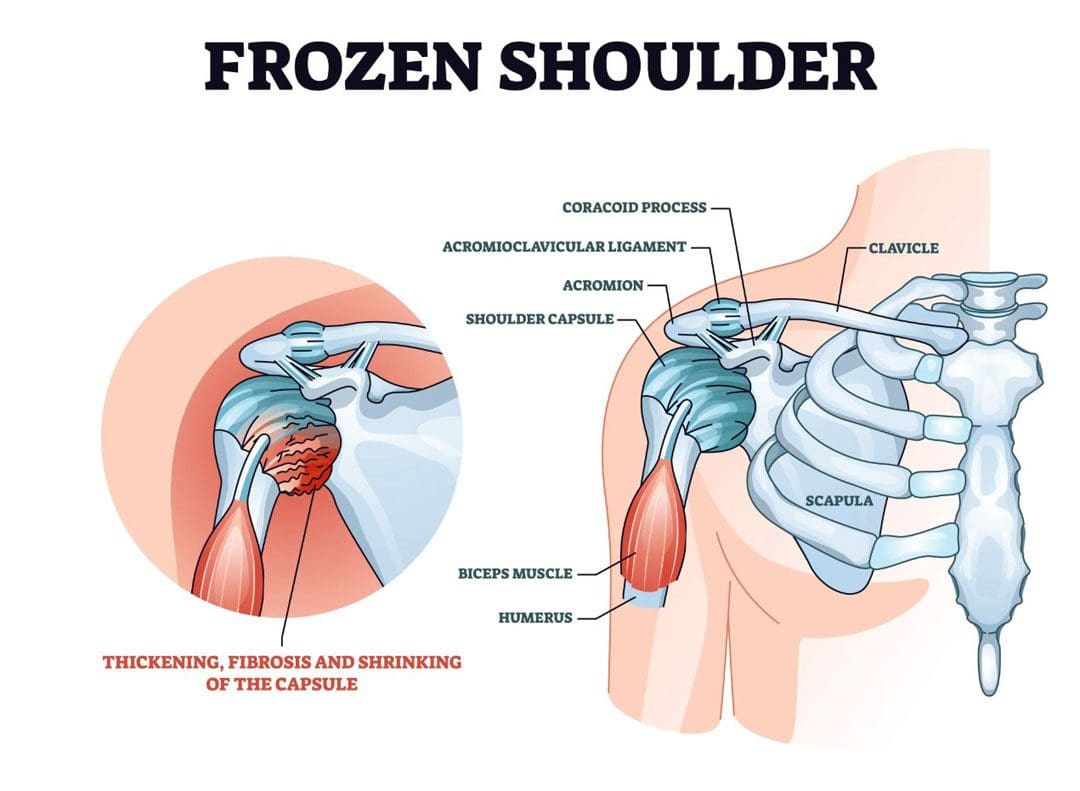
Table of Contents
Stiffness and Pain
The shoulder joint allows more movement than any other joint in the body. A frozen shoulder causes the capsule surrounding the shoulder joint to contract and form scar tissue. The capsule contraction and the formation of adhesions cause the shoulder to become stiff, restrict movement, and cause pain and discomfort symptoms.
Stages
The progression is marked by three stages:
Freezing
- Stiffness and pain begin to restrict motion.
Frozen
- Movement and motion are severely restricted.
Thawing
- The shoulder starts to loosen up.
- It can take years to fully resolve symptoms.
- In mild cases, a frozen shoulder can go away on its own but that does not mean that it is truly healed and correctly aligned.
- Even in mild cases seeking treatment is recommended, rather than just waiting for it to go away.
Symptoms
- Limited range of motion.
- Stiffness and tightness.
- Dull or aching pain throughout the shoulder.
- Pain can radiate into the upper arm.
- Pain can be triggered by the smallest movements.
- The symptoms are not always due to weakness or injury, but actual joint stiffness.
Causes
Most frozen shoulders occur with no injury or discernible cause but the condition is often linked to a systemic condition or one that affects the entire body.
Age and Gender
- Frozen shoulder most commonly affects individuals between the ages of 40 to 60, and is more common in women than in men.
Endocrine Disorders
- Individuals with diabetes have an increased risk of developing a frozen shoulder.
- Other endocrine abnormalities like thyroid problems can also lead to the development of this condition.
Shoulder Trauma and/or Surgery
- Individuals who sustain a shoulder injury, or undergo surgery on the shoulder can develop a stiff and painful joint.
- When injury or surgery is followed by prolonged immobilization/resting the arm, the risk of developing a frozen shoulder increases.
Other Systemic Conditions
Several systemic conditions such as heart disease have also been associated with an increased risk of developing the condition and can include:
- High cholesterol
- Adrenal disease
- Heart and lung disease
- Parkinson’s disease
Stiffness and pain can also be associated with damage to the joint from injuries or other shoulder problems that include:
- Muscle or connective tissue injury
- Rotator cuff tendinopathy
- Calcific tendinitis
- Dislocation
- Fracture
- Osteoarthritis
- A frozen shoulder associated with any of these causes is considered secondary.
Treatment
A diagnosis is made by observing the range of motion in the shoulder, considering the two types:
Active Range
- This is how far an individual can move a body part on their own.
Passive Range
- This is how far another person like a therapist or doctor can move the body part.
Therapies
- Chiropractic, massage, and physical therapy involve stretches, realignment, and exercises to relieve pain symptoms and restore mobility and function.
- Usually, strength is not affected by a frozen shoulder but a chiropractor may want to strengthen the surrounding muscles to better support the shoulder and prevent worsening the injury or causing a new injury.
- Anti-inflammatory medications and corticosteroid injections may help manage pain symptoms.
- Getting a diagnosis and treatment during the freezing stage can keep the condition from progressing and expedite recovery time.
Enhancing Health: Evaluation and Treatment
References
Brun, Shane. “Idiopathic frozen shoulder.” Australian Journal of general practice vol. 48,11 (2019): 757-761. doi:10.31128/AJGP-07-19-4992
Chan, Hui Bin Yvonne, et al. “Physical therapy in the management of frozen shoulder.” Singapore medical journal vol. 58,12 (2017): 685-689. doi:10.11622/smedj.2017107
Cho, Chul-Hyun, et al. “Treatment Strategy for Frozen Shoulder.” Clinics in orthopedic surgery vol. 11,3 (2019): 249-257. doi:10.4055/cios.2019.11.3.249
Duzgun, Irem, et al. “Which method for frozen shoulder mobilization: manual posterior capsule stretching or scapular mobilization?.” Journal of Musculoskeletal & neuronal interactions vol. 19,3 (2019): 311-316.
Jain, Tarang K, and Neena K Sharma. “The effectiveness of physiotherapeutic interventions in the treatment of frozen shoulder/adhesive capsulitis: a systematic review.” Journal of back and musculoskeletal rehabilitation vol. 27,3 (2014): 247-73. doi:10.3233/BMR-130443
Kim, Min-Su, et al. “Diagnosis and treatment of calcific tendinitis of the shoulder.” Clinics in shoulder and elbow vol. 23,4 210-216. 27 Nov. 2020, doi:10.5397/cise.2020.00318
Millar, Neal L et al. “Frozen shoulder.” Nature reviews. Disease primers vol. 8,1 59. 8 Sep. 2022, doi:10.1038/s41572-022-00386-2
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card



Comments are closed.