Spinal Tap: Diagnose, Administer Medicine, and Imaging
Most of us have heard the term spinal tap, or have seen it on a tv medical drama show. It is known as a lumbar puncture, but what does this procedure involve and how is it utilized? What to know. This procedure is performed in the lower part of the back. It can be used for:
- Health diagnosis
- Medication administration
- Imaging assistance
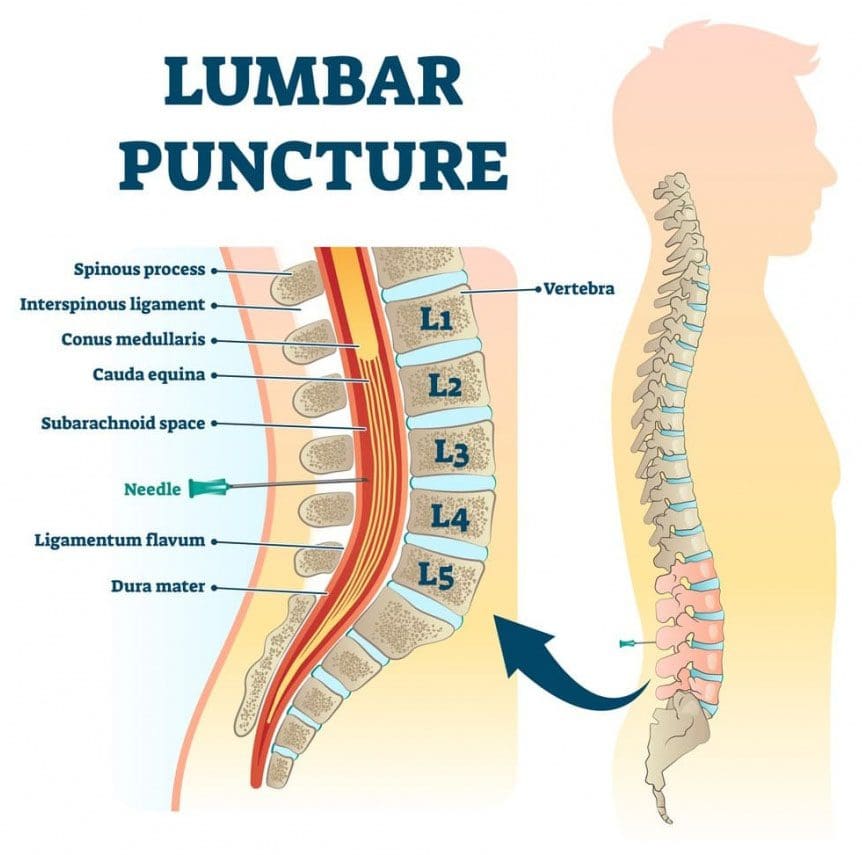
A spinal tap is performed by a doctor or nurse trained to do lumbar punctures. A specialized needle is inserted between the vertebrae to collect cerebrospinal fluid. Cerebrospinal fluid is a watery, colorless fluid that cushions the spinal cord and brain, protecting them from injury/damage. Questions may arise as to when an individual would need a spinal tap, how dangerous it is, and what to expect from this procedure?

Table of Contents
Spinal Tap Utilization
Spinal taps are often utilized in helping to diagnose infections of the central nervous system. One of the most common infections is meningitis. A sample of cerebrospinal fluid is taken, tested, and if infectious organisms are growing within, these are clue/s for determining and customizing a treatment plan and antibiotic therapy. The procedure also helps with:
- Identifying central nervous system disorders, like multiple sclerosis, or epilepsy for example.
- Diagnosing cancers that affect the brain or spinal cord
- Administration of chemotherapy or anesthesia
Spinal taps are also used with imaging assistance.
For example, a contrast dye can be injected into the cerebrospinal fluid to get an anatomical view of the spinal cord and coverings. They are quite helpful when an individual cannot have an MRI done.
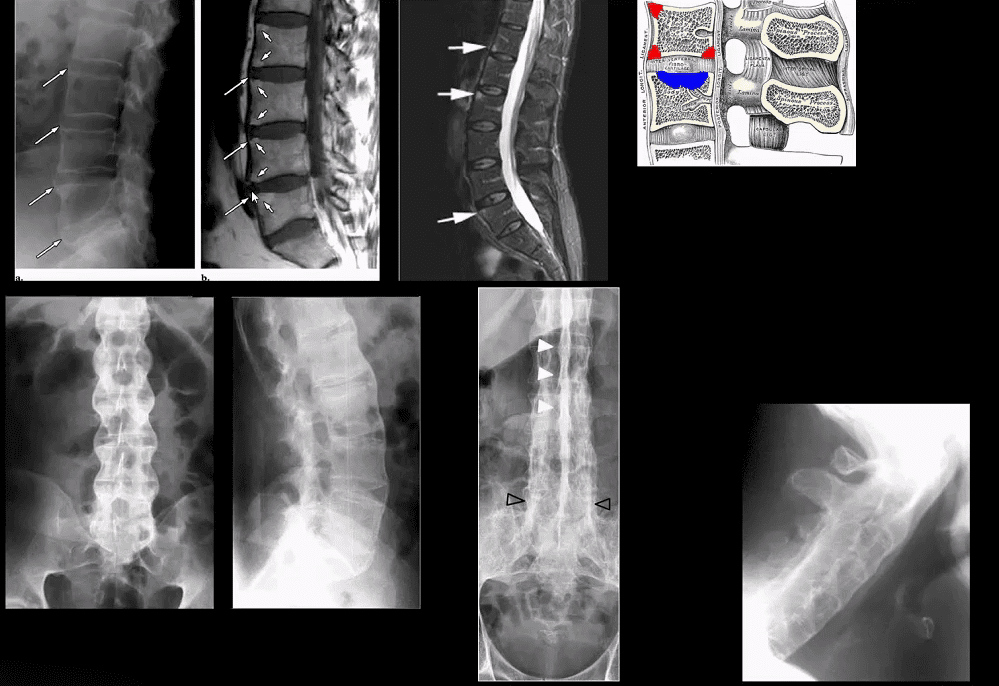
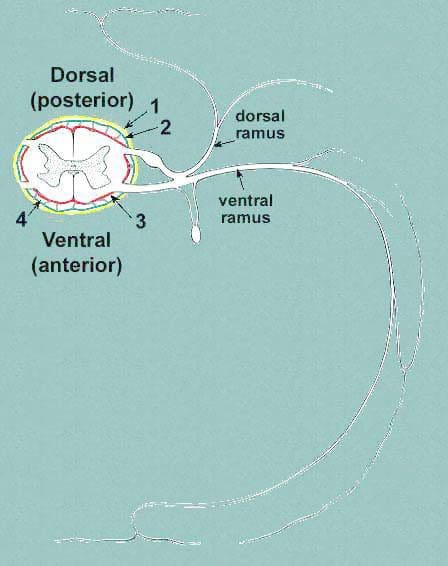
Spinal cord coverings from a cross-section of a nerve
Spinal cord rear view
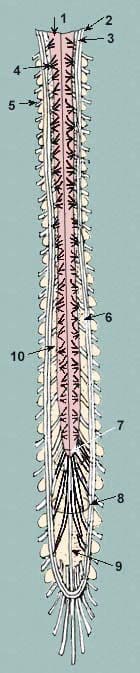
- spinal cord
- arachnoid
- dorsal rootlets of the
- spinal nerve
- the spinal nerve of
- the posterior surface of the body of the vertebra
- conus medullaris
- cauda equina
- filum terminale
- subarachnoid space
A spinal tap is done in a hospital or outpatient facility, depending on the reason for the tap. It is not an emergency procedure. Emergencies bring to mind situations and events that have to be done within seconds/minutes. A lumbar puncture does not entail that type of action.
Preparation
Listen and follow the provider’s instructions regarding what to eat and drink.
- An individual could be told to not eat or drink anything for a specific set of hours before.
- Any prescription/s, over-the-counter meds, and drug allergies need to be disclosed to the medical team that will perform the procedure.
- Individuals can wear their own clothes but preferably loose-fitting and comfortable should be the objective.
- Once at the location a hospital gown is given to the patient for the procedure.
- On the day of the appointment, tell the doctor of any unusual symptoms.
- Have a designated driver for the ride home, as sometimes a patient can feel weak and dizzy after the procedure.
The Procedure
A tap is a simple procedure that usually takes a half-hour or less to complete.
- The patient sits bent forward or lying down on the side.
- The knees should be pulled up as far as possible with the chin down into the chest curled into a ball.
- This arcs the back and spaces out the vertebrae, so there is a wider area for the needle to enter.
- The skin is cleaned with an antiseptic.
- A sterile sheet or towel is placed over the patient that has an opening exposing the lower back.
- Local anesthesia is injected to numb the area.
- Unless the doctor instructs movement, remaining still is key as the advancement of the needle into the small area is a delicate procedure.
- There is an initial what feels like a stinging sensation, but the patient does not feel the actual needle as it advances.
- The needle gets inserted into the spinal space where the cerebrospinal fluid resides.
- The cerebrospinal fluid pressure is measured.
- Sometimes an ultrasound or specialized x-ray technique, known as fluoroscopy is used to locate the best place for the needle.
- This is where the reason for the tap determines what action is taken. Either medicine is administered or a small amount of cerebrospinal fluid is taken.
- The needle is retracted.
- A bandage is applied.
- Spinal tap pain is rare, but sometimes the needle can brush a nerve root when it is inserted. It could feel like an electric shock down the leg.
Recovery
Once finished, the patient lies on their back for 30 to 60 minutes so the doctor can check for any abnormalities or effects. Being sent home depends on the reason for the tap. If there is unexplained fever, nausea, etc, a patient will not be sent home.
If it was an outpatient procedure the patient can leave and resume some simple activities after having a few hours of relaxation. Temporary pain meds are prescribed to address any discomfort. Results could come a day or a week later. They depend on the reason for the spinal tap.
Risks and Complications
It is considered a safe procedure with rare complications. The most common effect is a headache which usually comes on several hours, to a day or two later. These will not lead to any neurologic problems. Water or tea can help prevent and reduce headaches. Over-the-counter pain relievers can help too. However, if the headache continues after two days, call the doctor. A very small possibility of a more severe complication could happen including:
- Infection
- Bleeding
- Numbness
- Brain herniation or movement of the brain tissue from the added pressure
- Nerve or spinal cord damage
This is a very safe procedure with the medical team being highly trained and skilled professionals that are careful and gentle.
Auto Accident Doctors & Chiropractic Treatment
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card



Comments are closed.