For older individuals, experiencing frequent low back pain could turn out to be a sacral fracture. They tend to occur in individuals over the age of 60 often because there has been a degree of bone loss. Sacral fractures tend not to be the first thing doctors think of when low back pain symptoms are presenting. They are often not picked up on X-rays and are either not diagnosed early enough to take steps or not diagnosed at all. However, they are common.
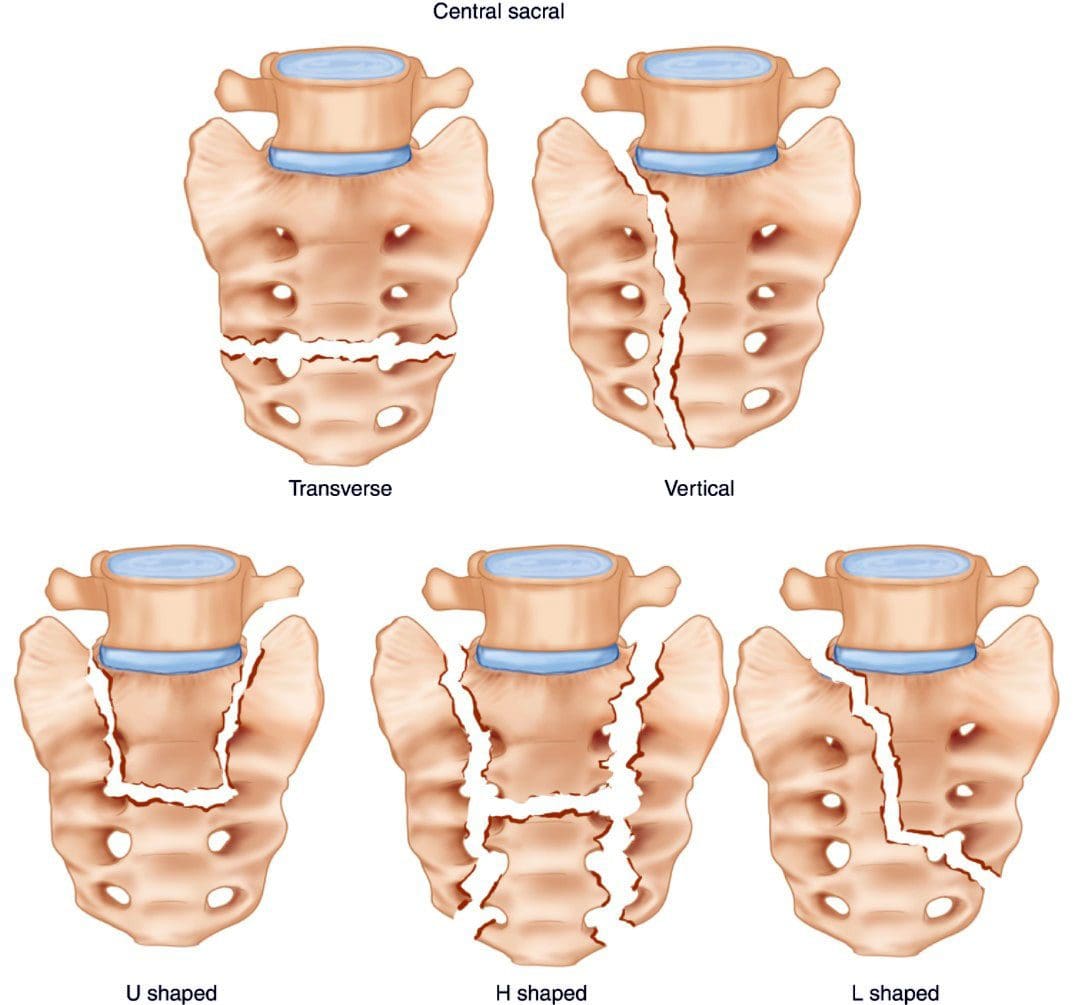
Table of Contents
Sacrum
The sacrum is shaped like a triangle and comprises five segments fused into one large bone. It sits at the base of the spine, between the two halves of the pelvis, connecting the spine to the lower half of the body. It stabilizes the body when walking, sitting, or standing. The nerves in the lower spine control the bowels bladder and provide sensation to the region.
- The two dimples that can be seen on individuals’ backs are where the sacrum joins the hipbones or the sacroiliac joint.
- The point where the low back joins the sacrum can develop discomfort, soreness, and pain.
- This area experiences stress from bending, twisting, reaching, lifting, carrying during physical activities or sitting for long periods.
Sacral Fracture
Most sacral fractures result from trauma, like slips, falls, and automobile accidents. Stress fractures that happen without a specific injury are also called insufficiency fractures.
Types of Sacral Fractures
- Low-energy fractures usually happen to older individuals with weak bones due to osteoporosis.
- An individual trips on something, lands hard on their butt, lifts a heavy object awkwardly, or over-exerts themselves from some physical activity.
- Then persistent back or buttock pain begins to present.
- The pain is often centered in the lower back, the hips, and butt.
- It is more than just back achiness.
- The individual goes to the doctor, and X-rays are ordered.
- A lot of the time, these fractures are missed on X-rays.
- The doctor may diagnose a sprain, but the pain symptoms do not improve.
- Sometimes there is no apparent cause for the pain.
- It can be misdiagnosed as a lower back compression fracture or urinary tract infection.
- High-energy fractures are due to trauma and are more common among the young.
- The individual sustains injuries from an auto accident, has fallen from a significant height, or suffers a sports injury.
- It results in severe pain.
- A woman who has just had a baby and gone through some bone loss because of the pregnancy can experience a sacral stress fracture.
Diagnosis
The most common causes for low back pain include:
- Frequent improper posture.
- Muscle weakness or tightness.
- Ligament strain.
- Joint inflammation.
- A pilonidal cyst or an anal fissure can also cause pain.
For individuals that have been to a doctor and had an X-ray that reveals no fracture, and there is no improvement after 5 to 7 days, it is recommended to schedule another appointment and ask for a CAT scan or MRI, which is highly effective at finding a sacral fracture.
Treatment
Treatment consists of resting the bone but still being safely active in most cases.
- Medication is prescribed for pain relief.
- Many individuals have been found to do well with anti-inflammatory medications, topical medications, and lidocaine patches.
- Older individuals may be recommended to use a walker during the treatment/healing process.
- Depending on the severity, crutches may be recommended.
- Engaging in regular exercise is not recommended, but too much bed rest is also not recommended.
- Too much rest may not allow the injury to heal correctly, worsen the injury, and/or cause new injuries.
- Chiropractic and physical therapy are not recommended to let the sacrum naturally heal.
- After the pain subsides, chiropractic and physical therapy can be implemented to maintain agility and flexibility and strengthen the pelvic and core muscles.
In some cases, if the bone does not heal correctly or some other issue, sacroplasty could be recommended. This is a minimally invasive procedure that injects bone cement into the fracture. It offers quick and long-lasting pain relief with a low percentage of complications. It is considered low risk and can be done by an interventional radiologist or spine surgeon.
Prevention
To minimize the risk of a sacral fracture, it is highly recommended to maintain bone strength. This consists of:
- Having a balanced diet.
- Eating calcium-rich foods.
- Taking calcium and vitamin D supplements.
- Strength training.
- Regular bone density screenings.
Body Composition
Sitting Posture Adjustments
Adjust Sitting
- If allowed, sit on an exercise ball for short periods, or try a sit-stand desk. There are also treadmill desks and bicycle desks.
- If none of these are possible options, try exercises to do at a desk that works out the core muscles.
Change Chair
- Try a solid wooden chair if unable to use a ball or sit-stand desk.
- It will make the body sit up straight and increase proper posture.
Move Around Alarm
- Set a timer every hour for two minutes of movement.
- Try to keep moving with different exercise stretches, or take a lap around the building.
References
Gibbs, Wende Nocton, and Amish Doshi. “Sacral Fractures and Sacroplasty.” Neuroimaging clinics of North America vol. 29,4 (2019): 515-527. doi:10.1016/j.nic.2019.07.003
Holmes, Michael W R, et al. “Evaluating Abdominal and Lower-Back Muscle Activity While Performing Core Exercises on a Stability Ball and a Dynamic Office Chair.” Human factors vol. 57,7 (2015): 1149-61. doi:10.1177/0018720815593184
Santolini, Emmanuele et al. “Sacral fractures: issues, challenges, solutions.” EFORT open reviews vol. 5,5 299-311. 5 May. 2020, doi:10.1302/2058-5241.5.190064
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card



Comments are closed.