[et_pb_section bb_built=”1″][et_pb_row][et_pb_column type=”4_4″][et_pb_text]
A migraine is commonly identified by a moderate to severe throbbing pain or a pulsing sensation, usually on one side of the head, often accompanied by nausea, vomiting and extreme sensitivity to light and sound. Migraine headache pain can last for hours to even days and the symptoms can become so severe they may be disabling. Many doctors can treat varying intensities of head pain, however, the use of drugs and/or medications may only temporarily relieve the painful symptoms. Evidence-based research studies like the one described below, have determined that chiropractic spinal manipulative therapy may effectively improve migraine headaches. The purpose of the article is to educate patients on migraine headache chiropractic treatment.
Table of Contents
A Twelve Month Clinical Trial of Chiropractic Spinal Manipulative Therapy for Migraine
Abstract
- Objective: To assess the efficacy of Chiropractic spinal manipulative therapy (SMT) in the treatment of migraine.
- Design: A prospective clinical trial of twelve months duration. The trial consisted of 3 stages: two month pre- treatment, two month treatment, and two months post treatment. Comparison of outcomes to the initial baseline factors was made and also 6 months after the cessation of the study.
- Setting: Chiropractic Research Centre of Macquarie University
- Participants: Thirty two volunteers, between the ages of 20 to 65 were recruited through media advertising. The diagnosis of migraine was based on a self reported detailed questionnaire, with minimum of one migraine per month.
- Interventions: Two months of chiropractic SMT at vertebral fixations determined by the practitioner, through orthopedic and chiropractic testing.
- Main Outcome Measures: Participants completed diaries during the entire trial noting the frequency, intensity (visual analogue score), duration, disability, associated symptoms and use of medication for each migraine episode.
- Results: The initial 32 participants showed statistically significant (p < 0.05) improvement in migraine frequency, VAS, disability, and medication use, when compared to initial baseline levels. A further assessment of outcomes after a six month follow up (based on 24 participants), continued to show statistically significant improvement in migraine frequency (p < 0.005), VAS (p < 0.01), disability (p < 0.05), and medication use (p < 0.01), when compared to initial baseline levels. In addition, information was collected regarding any changes in neck pain following chiropractic SMT. The results indicated that 14 participants (58%) reported no increase in neck pain as a consequence of the two months of SMT. Five participants (21%) reported a slight increase, three participants (13%) reported mild pain, and two participants (8%) reported moderate pain.
- Conclusion: The results of this study support the hypothesis that Chiropractic SMT is an effective treatment for migraine, in some people. However, a larger controlled study is required.
- Key Indexing Terms (MeSH): Migraine; chiropractic; spinal manipulation; prospective trial; neck.
Introduction
The cervical spine as a cause of headache has been well described in the literature (1,2). The Headache Classification Committee of the International Headaches Society, has defined cervicogenic headache, in addition to the other types of headaches, including migraine and tension type headache (3).
However, the role of spinal conditions (especially the cervical spine) and their associated treatment for migraine does not have a well established causal relationship or clear aetiological pathway (4-7). In addition, migraine often has uncertain or overlapping diagnostic criteria thus making the role of the cervical spine as an aetiological factor even more uncertain (8,9).

Migraines are a common and debilitating conditions yet because of this uncertain aetiology, the most appropriate long term treatment has not been established (9,10). Most aetiological models relate to vascular causes of migraine, where episodes seem to be initiated by a decreased blood flow to the cerebrum followed by extracranial vasodilatation during the headache phase (11,12). However, other aetiological models seem connected with vascular changes related to neurological causes and associated serotonergic disturbances (10). Therefore, previous treatments have focused on pharmacological modification of blood flow or serotonin antagonist block (11).
This paper will evaluate the efficacy of chiropractic spinal manipulative treatment during a prospective clinical trial of twelve months duration.
Chiropractic Treatment
Chiropractic SMT is defined as a passive manual manoeuvre during which the three joint complex is carried beyond the normal physiological range of movement without exceeding the boundaries of anatomical integrity (4). SMT requires a dynamic force in a specific direction, usually with a short amplitude to correct a problem of reduced vertebral motion or positional fault. Treatment usually consists of short amplitude, high velocity spinal manipulative thrusts (diversified technique), on areas of vertebral fixation determined by a clinical history and physical examinations.

The most commonly used factors to locate vertebral fixation (denoted vertebral subluxation complex by chiropractors) are a clinical history relating to mechanical pain patterns and medical details to excluded possible non- mechanical causes (4). These findings would then be confirmed by a thorough physical examination, by assessing which tests/signs (orthopaedic and chiropractic) were able to reproduce the presenting symptom (7).
Studies in effectiveness and cost-effectiveness of treatment for back pain have found significant benefit for chiropractic spinal manipulative therapy (SMT). These studies have been detailed in a previous publication by this author on chiropractic in the workers compensation system (13). In addition, numerous studies have identified improvement in neck pain and headache following chiropractic SMT (4,7,14-17).
This paper will test an hypothesis that spinal conditions appear to contribute to the aetiology and morbidity of migraine.
Methodology
The study was twelve month prospective clinical trial which involved 32 subjects who received a two month course of chiropractic SMT. Treatment consisted of short amplitude, high velocity spinal manipulative thrusts (chiropractic adjustive technique), on areas of vertebral subluxation determined by the physical examination.
Participants were recruited via the radio and newspapers in the Sydney region. Applicants completed a previously reported questionnaires, and were selected according to responses in the following symptoms. The participants needed to a minimum of 5 of the following IHS indicators: reaction to pain requiring cessation of activities, the need to seek a quiet dark area, unilateral pain located parieto- temporal, pain described as pulsating/throbbing, associated symptoms of nausea &/or vomiting, photophobia &/or phonophobia, migraine aggravated by head or neck movements, and a family history of migraine (3).
Inclusion was also based on participants experiencing at least one migraine a month. Exclusion was based on non- migraine indicators of a daily migraine or the initiating factor being trauma. Participants were also excluded from the study if there were contra-indications to SMT, such as meningitis or cerebral aneurysm. In addition, participants with temporal arteritis, benign intracranial hypertension or space occupying lesions were also excluded due to safety aspects.
Participants completed diaries during the initial six month trial noting the frequency, VAS, duration, disability, associated symptoms and use of medication for each migraine episode. Participants were instructed how to complete the diary which contained a table and an instruction sheet. Participants had to note the date of the migraine, an intensity score based on a visual analogue scale, the hours the migraine lasted and the time before they could return to normal activities. In addition, participants noted associated symptoms using a letter abbreviation and they noted the type and strength of medication for each migraine episode.
Patient’s blinding was achieved by participants being informed that they may be randomly assigned to a control group which would receive a placebo (non effective) treatment. Concurrently, the practitioners were “blinded” to previous treatment results, assignment of control procedures and other outcome measures.
The first aspect of the trial was conducted over six months, and consisted of 3 stages: two months pre-treatment, two months treatment, and two months post treatment. Participants were contacted by the author a further six months after the initial trial and asked to complete another questionnaire regarding their current migraine episodes for comparison to baseline data. The follow up questionnaire sought information on the same outcome measures, as detailed in the diaries described above.
Comparison was made to initial baseline outcome measurements of migraine preceding commencement of SMT, data at the end of the two months post SMT, and to the six month follow up data. Statistical analysis involved comparing the changes of the different outcome measurements of frequency, VAS, duration, disability, and medication use throughout the trial. Statistical tests employed were a paired t test to test for significant difference between each group and a one way analysis of variance (ANOVA) to test for changes for all groups.
Dr. Alex Jimenez’s Insight
“How can chiropractic spinal manipulative therapy help manage my migraine headache pain?” Although researchers today don’t know the definitive cause behind these complex headaches, many healthcare professionals believe migraines are often the result of an underlying issue along the cervical spine, or neck. If you suffer from migraine headache pain, chiropractic treatment can help correct spinal misalignments, or subluxations, in the cervical spine to improve the severity of the headache and decrease their frequency. It’s not necessary to rely on drugs and/or medications to relieve the painful symptoms, however, these may be used if properly directed by a healthcare professional. Rather than focusing on the head pain alone, a doctor of chiropractic will target the source of the issue and help improve your overall health and wellness.
Results
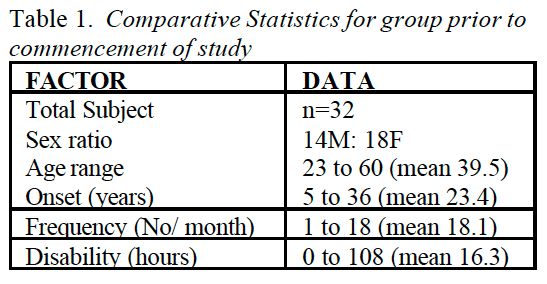
Thirty two participants, between the ages of 23 to 60, joined the study with there being 14 males and 18 females. Table 1 gives the comparative descriptive statistics for the group. The length of time the person had migraines ranged between 5 to 36 years for the group, with the average being 18.1 years. The duration of a typical migraine episode ranged between 0.75 to 108 hours for the group, with the average being 23.3 hours. The disability (length of time before the person could return to normal activities) of a typical migraine ranged between 0 to 108 hours for the group, with the average being 25.0 hours.
The percentage response for each of the diagnostic criteria of the IHS guidelines is detailed in table 2 (Table 2). The highest responses were for photophobia (91%), nausea (88%), reaction to pain requiring the person to seek a quiet dark area (84%), phonophobia (72%), throbbing pain characteristic (69%), parieto-temporal pain location (69%), inability to continue normal activities (66%), and family history (63%).
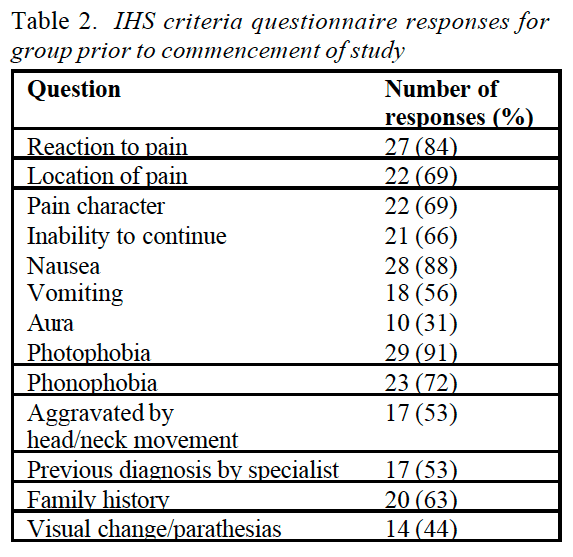
The IHS diagnostic criteria with the lowest responses were aura (31%), migraines aggravated by head or neck movement (53%), and vomiting (56%). A moderate number (44%) of people did not indicate aura as a feature, however, they described either homonymous visual changes or parasthesias. Therefore, the number of people experiencing migraine with aura (MA) for this group was twenty four (75%) of a total group of thirty two.
The group showed statistically significant improvement (p < 0.05) in migraine frequency, VAS, duration and disability, when compared to initial baseline levels. The frequency rates reduced by 46% for the group, severity reduced by 12%, duration reduced by 20%, disability reduced by 14% only one participant (3.1 %) reported that their migraine episodes were worse after the two months of SMT, but this was not sustained at the two month post treatment follow up period. Table 3 demonstrates variate scores in each of the six diary categories for the three phases of the trial.
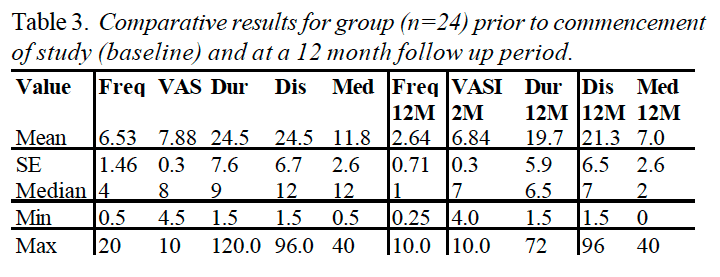
From the initial thirty two participants who entered the study, four participants failed to complete the entire trial, one due to alteration in work situation, one due to a fractured ankle, one due to soreness after SMT, and one ACO following a perceived worsening of their migraine due to chiropractic SMT. In addition, four people failed to return their six month follow up data, and were excluded from the assessment. Therefore the assessment of changes in migraine at the twelve month period was based on 24 participants. Table 4 gives the comparative statistics for this group at the end of the 12 month period.
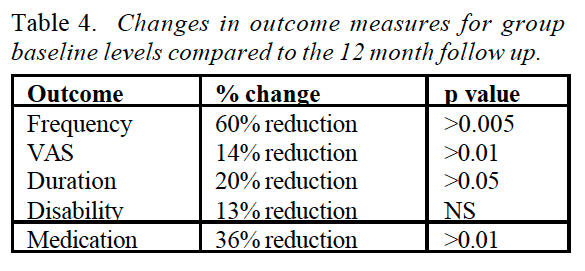
The average response at twelve months (n=24) showed statistically significant improvement in migraine frequency (p < 0.005), VAS (p < 0.01), duration (p < 0.05), and medication use (p < 0.01), when compared to initial baseline levels (Figure ????). The greatest area for improvement was with the frequency of episodes (60% reduction), and the associated severity of each migraine (14% reduction). In addition, the duration of the migraine (20% reduction) and the use of medication, reduced significantly following the SMT intervention (36% reduction). Table 3 shows mean variate scores for the three phases of the trial and statistical significance by analysis of variance (ANOVA).
Another additional result related to associated neck pain. Fourteen participants (58%) reported no increase in neck pain as a consequence of the two months of SMT. Five participants (21%) reported slight pain, three participants (13%) reported mild pain, and two participants (8%) reported moderate pain.
Discussion
The majority of participants were chronic migraine sufferers, on average they had experienced migraines for 18.1 years. However, the results have demonstrated a significant (p< 0.005) reduction in their migraine episodes and their associated disability. The mean number of migraines per month reduced from 7.6 to 2.6 episodes.
A twelve month study gives the results substantial significance because a criticism of early studies were that the length of the trial was too short to allow for the cyclical nature of migraines (18). However, the study was limited in the sample size and the fact that the trial was a pragmatic study which did not consider what aspects of chiropractic SNIT had contributed to the improvement in the migraines.
In addition, the study was limited due to the lack of a control group. However, it could be argued that participants acted as their own form of control, due to the baseline two months data collection, especially given the fact that this group were chronic migraine sufferers.
A further limitation of this study, as with other studies of migraine or headaches was that there is substantial overlap in diagnosis and classification of migraines. The questionnaire used in this study proved to have good reliability, however, there is strong suggestion that many headache sufferers may have more than one type of headache (6-9). An advantage with the design of this study is that regardless of the exact “diagnosis” of the migraine, self reported improvement of outcome measures allow assessment of the validity of the therapy in question (4).
This study appears to confirm that there are a number of precipitating or aggravating factors involved in migraine episodes and therefore a single treatment regime may prove ineffective in the long term (4,5,9,15).
Practitioners need to be aware of the various treatment strategies and their relative advantages or limitations.
Importantly, many of the associated symptoms suffered by participants on the trial were reported to be decreased following the SMT. The associated symptoms which decreased following the trial included nausea (41% of participants felt reduction), photophobia (31 % felt reduction), vomiting (25% felt reduction), and phonophobia (25% felt reduction). Commonly reported side effects which often increase following pharmaceutical trials include nausea, vomiting, fatigue, chest pain, paraesthesia, somnolence, syncope, vertigo and less commonly atrial fibrillation. In addition, recent evidence has identified sumatriptan to be a potential cause of birth defects and myocardial infarction (19,20).

Whilst not a factor noted by the IHS, stress as either an aggravating or precipitating factor was cited by 73% of participants. In addition, 66% of people reported neck pain at the time of the migraine, with a further 31 % of people reporting upper back pain (some people noted both simultaneously).
Interestingly, five people at the end of the 12 months followup had no migraines and had decreased need for medication by 100% following chiropractic SMT. No patients reported that their migraines had increased as a result of the SMT trial.
Conclusion
The results of this study support the hypothesis that Chiropractic SMT is an effective treatment for migraine, in some people. However, due to the multifactorial nature of migraine, and the finding that episodes usually reduce following any intervention, further larger controlled study is required.
A prospective randomised controlled trial utilising detuned EPT (interferential), a sham manipulation group and an SMT group is nearing conclusion. It is anticipated this trial will provide further information of the efficacy of Chiropractic SMT in the treatment of migraine with aura.
In conclusion, because migraine headache pain can be significantly debilitating, it’s essential for patients who suffer from this complex type of head pain to understand the effectiveness of chiropractic spinal manipulative therapy. According to the results of the research study above, migraine headache chiropractic treatment can be effectively used to as migraine treatment. Regardless of the results of the twelve month clinical trial, further research studies are still required. Information referenced from the National Center for Biotechnology Information (NCBI). The scope of our information is limited to chiropractic as well as to spinal injuries and conditions. To discuss the subject matter, please feel free to ask Dr. Jimenez or contact us at 915-850-0900 .
Curated by Dr. Alex Jimenez

Additional Topics: Neck Pain
Neck pain is a common complaint which can result due to a variety of injuries and/or conditions. According to statistics, automobile accident injuries and whiplash injuries are some of the most prevalent causes for neck pain among the general population. During an auto accident, the sudden impact from the incident can cause the head and neck to jolt abruptly back-and-forth in any direction, damaging the complex structures surrounding the cervical spine. Trauma to the tendons and ligaments, as well as that of other tissues in the neck, can cause neck pain and radiating symptoms throughout the human body.

IMPORTANT TOPIC: EXTRA EXTRA: A Healthier You!
OTHER IMPORTANT TOPICS: EXTRA: Sports Injuries? | Vincent Garcia | Patient | El Paso, TX Chiropractor
[/et_pb_text][et_pb_accordion _builder_version=”3.0.105″][et_pb_accordion_item _builder_version=”3.0.105″ title=”Blank” use_background_color_gradient=”off” background_color_gradient_start=”#2b87da” background_color_gradient_end=”#29c4a9″ background_color_gradient_type=”linear” background_color_gradient_direction=”180deg” background_color_gradient_direction_radial=”center” background_color_gradient_start_position=”0%” background_color_gradient_end_position=”100%” background_color_gradient_overlays_image=”off” parallax=”off” parallax_method=”on” background_size=”cover” background_position=”center” background_repeat=”no-repeat” background_blend=”normal” allow_player_pause=”off” background_video_pause_outside_viewport=”on” text_shadow_style=”none” box_shadow_style=”none” custom_css_main_element=”display:none;” /][et_pb_accordion_item _builder_version=”3.0.105″ title=”References” use_background_color_gradient=”off” background_color_gradient_start=”#2b87da” background_color_gradient_end=”#29c4a9″ background_color_gradient_type=”linear” background_color_gradient_direction=”180deg” background_color_gradient_direction_radial=”center” background_color_gradient_start_position=”0%” background_color_gradient_end_position=”100%” background_color_gradient_overlays_image=”off” parallax=”off” parallax_method=”on” background_size=”cover” background_position=”center” background_repeat=”no-repeat” background_blend=”normal” allow_player_pause=”off” background_video_pause_outside_viewport=”on” text_shadow_style=”none” box_shadow_style=”none”]
1. Bogduk N. Cervical causes of headache and dizziness. In: Greive GP (ed) Modern manual therapy of the vertebral column. 2nd ed 1994. Churchill Livingstone, Edinburgh. p3l7-31.
2. Jull GA. Cervical Headache: a review. In: Greive GP (ed) Modem manual therapy of the vertebral column. 2nd ed 1994. Churchill Livingstone, Edinburgh. p 333-34,6
3. Headache Classification Committee of the International Headache, Society. Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Cephalgia 1988, 9. Suppl. 7: 1-93.
4. Tuchin PJ. The efficacy of chiropractic spinal manipulative therapy (SMT) in the treatment of migraine – a pilot study. Aust Chiro & Osteo 1997; 6: 41-7.
5. Milne E. The mechanism and treatment of migraine and other disorders of cervical and postural dysfunction. Cephaigia 1989; 9, Suppi 10: 381-2.
6. Kidd R, Nelson C. Musculoskeletal dysfunction of the neck in migraine and tension headache. Headache 1993; 33: 566-9.
7. Tuchin PJ, Bonello R. Classic migraine or not classic migraine, that is the question. Aust Chiro & Osteo 1996; 5: 66-74.
8. Marcus DA. Migraine and tension type headaches: the questionable validity of current classification systems. 1992; Pain 8: 28-36.
9. Rasmussen BK, Jensen R, Schroll M, Olsen J. Interactions between migraine and tension type headaches in the general population. Arch Neurol 1992; 49: 914-8.
10. Lance JW. A concept of migraine and the search for the ideal headache drug. Headache 1990; 1: 17-23.
11. Dalassio D. The pathology of migraine. Clin J Pain 1990 6: 235-9.
12. Moskowitz MA. Basic mechanisms in vascular headache. Neurol Clin 1990; 16: 157-68
13. Tuchin PJ, Bonello R. Preliminary Findings of Analysis of Chiropractic Utilisation and Cost in the Workers Compensation System of New South Wales. J Manipulative Physiol Ther 1995; lg: 503-11.
14. Tuchin PJ, Scwafer T, Brookes M. A Case Study of Chronic Headaches. Aust Chiro & Osteo 1996; 5: 47-53.
15. Parker GB, Tupling H, Pryor DS. A Controlled Trial of Cervical Manipulation for Migraine. Aust NZ J Med 1978; 8: 585-93.
16. Young K, Dharmi M. The efficacy of cervical manipulation as opposed to pharmacological therapeutics in the treatment of migraine patients. Transactions of the Consortium for Chiropractic Research. 1987.
17. Vernon H, Steiman I, Hagino C. Cervicogenic dysfunction in muscle contraction headache and migraine: a descriptive study. J Manipulative Physiol Ther 1992; 15: 418-29
18. Parker GB, Tupling H, Pryor DS. Why does migraine improve during a clinical trial? Further results from a trial of cervical manipulation for migraine. Aust NZ J Med 1980; 10: 192-8.
19. Ottervanger JP, Stricker BH. Cardiovascular adverse reactions to sumatriptan: cause for concern? CNS Drugs 1995; 3: 90-8.
20. Simmons VE, Blakeborough P. The safety profile of sumatriptan. Rev Contemp Pharmacother 1994; 5: 319-28.
[/et_pb_accordion_item][et_pb_accordion_item _builder_version=”3.0.105″ title=”Close Accordion” use_background_color_gradient=”off” background_color_gradient_start=”#2b87da” background_color_gradient_end=”#29c4a9″ background_color_gradient_type=”linear” background_color_gradient_direction=”180deg” background_color_gradient_direction_radial=”center” background_color_gradient_start_position=”0%” background_color_gradient_end_position=”100%” background_color_gradient_overlays_image=”off” parallax=”off” parallax_method=”on” background_size=”cover” background_position=”center” background_repeat=”no-repeat” background_blend=”normal” allow_player_pause=”off” background_video_pause_outside_viewport=”on” open_toggle_background_color=”#ffffff” closed_toggle_background_color=”#ffffff” text_shadow_style=”none” custom_padding=”0px|||” custom_padding_tablet=”0px|||” custom_padding_phone=”0px|||” box_shadow_style=”none” custom_css_main_element=”border:none;” custom_css_toggle_title=”font-size:0.8em;” custom_css_toggle_icon=”display:none;” /][/et_pb_accordion][/et_pb_column][/et_pb_row][/et_pb_section]
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card


