Gluteus medius and minimus tendinopathy are painful and debilitating disorders in athletes. Chiropractor, Dr. Alexander Jimenez looks at the identification and rehabilitation options for this kind of injury…
No matter the condition that is overall of an athlete, the fact is that there are instances when their sport’s demands exceeds the movement and stability available during the kinetic chain of joints and the muscles utilized to execute that movement. Pattern compensation can occur if any weakness exists in almost any plane of motion and injury might be the outcome.
An illness that can arise from this and similar situations is gluteal tendinopathy (either medius or minimum). The mixture of overuse and inherent weakness of the gluteus medius and minimis can lead to stress, tearing, or degeneration of the muscles or their various tendons, inducing tendinopathy in the athlete.
Table of Contents
Hip Anatomy
A schematic view of gluteus medius and minimus can be viewed in Figure 1. The gluteus medius originates in the ilium inferior to the iliac crest and spans to the lateral and superior surfaces of the greater trochanter. Medius has two insertions: the superoposterior facet and the aspect. Of the two, the aspect includes a bigger area of insertion. Medius is a main hip abductor; the hip, while the posterior fibers help in external rotation is internally rotated by its anterior fibres. In weightbearing positions, these muscles keep the pelvis out of falling.
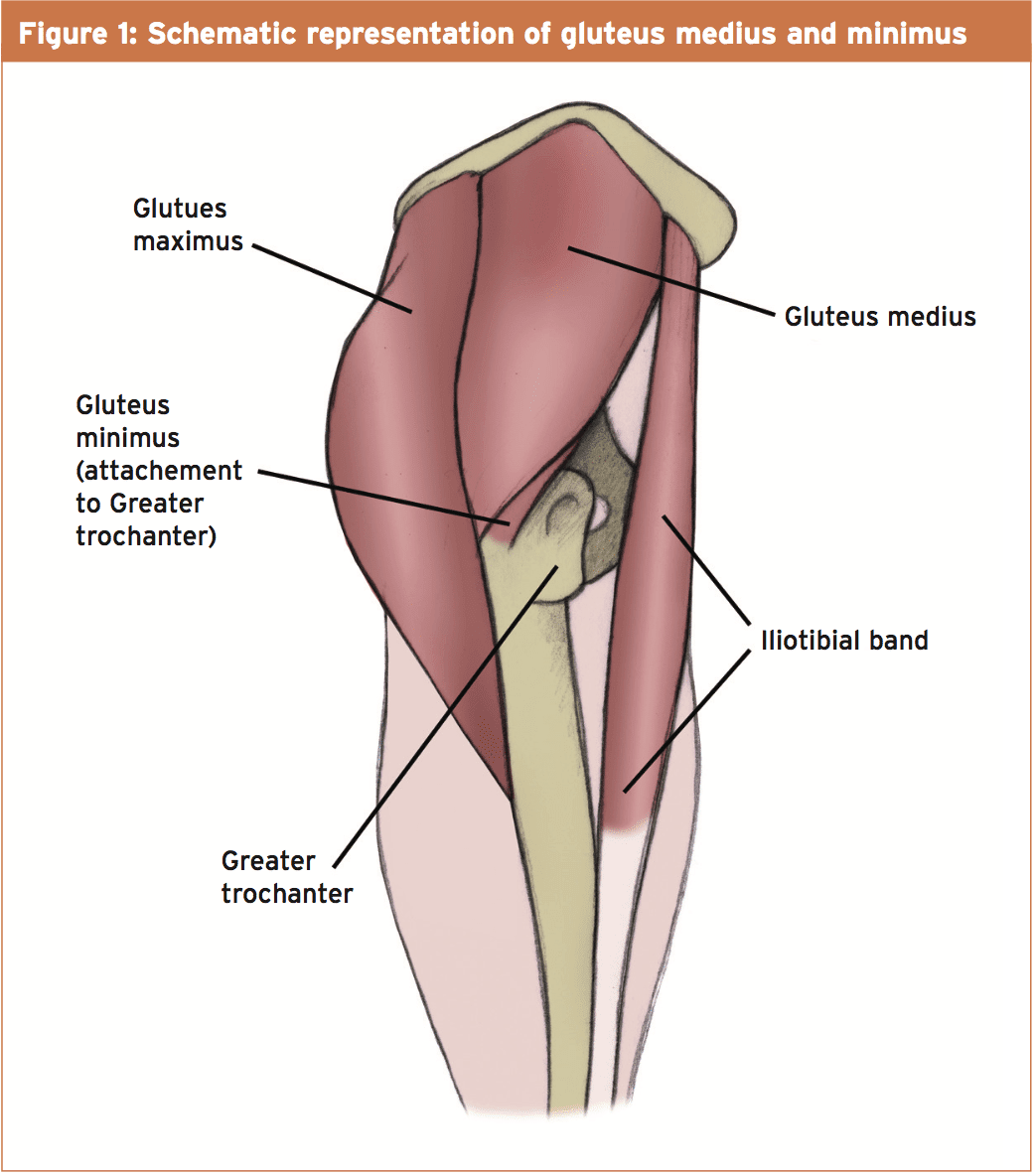 Gluteus minimus is a fan-shaped muscle lying to gluteus medius, and has the anterior and poor lines, as well as a source from the ilium and also the border of the greater sciatic notch. Gluteus minimus (in association with different muscles) chiefly abducts the hip when the hip is in extension and also a most important purpose of this muscle is to help reestablish the head of the femur in the acetabulum when an person is walking.
Gluteus minimus is a fan-shaped muscle lying to gluteus medius, and has the anterior and poor lines, as well as a source from the ilium and also the border of the greater sciatic notch. Gluteus minimus (in association with different muscles) chiefly abducts the hip when the hip is in extension and also a most important purpose of this muscle is to help reestablish the head of the femur in the acetabulum when an person is walking.
Indicators Of GlutealTtendinopathy
Tendinopathy is characterised by lateral hip pain in the shared insertion on the greater trochanter of the femur, and is often associated with higher trochanteric bursitis(1). Typically patients will complain of a dull and bronchial lateral hip pain, which can be aggravated abduction and by weight bearing under load.
To help distinguish the underlying muscular pathology (ie whether gluteus medius or minimus tendinopathy lies), medius tendinopathy often poses as tenderness along the anterior aspect of the greater trochanter in the tendinous insertion, whereas pain in the anterior part of the greater trochanter indicates the difficulties are more likely to be credited to gluteus minimus. In addition testing might be useful to help differentiate muscular from bursal pathology.
In some patients, however may present masquerading as other ailments, which then can lead to mismanagement and misdiagnosis of the condition. This is partly due to descriptions of the gluteus minimus are not always true and treatment protocols are not always unique to the pathology. Additionally, referred pain from the gluteus minimus can be acute as well as its source is relatively concealed; pain may be felt at the lateral and posterior element of the lower limb as far as the outer ankle and upward into the buttock, imitating sciatica(two). Palpation of the trigger point that is profound is not easy.
Diagnosis & Testing
When it comes to examining patients with suspected gluteal tendinopathy, a comprehensive and stepwise approach to the evaluation is recommended. This strategy should consist of taking a history from the patient, an inspection of the hip, palpation, followed by evaluations of range of movement, stability, and strength in all planes of motion. Areas and joints around the hip area (eg SI joint, lumbar spine) should also be analyzed. Gait patterns should be observed, noting any discrepancy and compensations due to weakness, in addition to heel strike and avoidance patterns. An MRI scan and/or ultrasound imaging is strongly suggested in case avulsion is suspected.
Unfortunately, there’s no definitive test to rule tendinopathy outside or in. But, there are quite a few different tests that can be quite helpful when assessing a patient. These are as follows:
- Trendelenburg test the functional power of gluteus medius. The patient stands unsupported on a single leg. If the pelvis tilts towards the unsupported leg, then this indicates abductor weakness about the stance leg;
- Ober’s test — that the individual lies on the unaffected hip. The symptomatic knee and hip have been held in a flexed position. The hip is abducted and long to centre the iliotibial band over the greater trochanter, and then passively adducted. Pain in This Procedure suggests a tight, contracted or inflamed tensor fasciae latae and iliotibial band;
- Thomas test — that the patient lies supine And retains the leg at the knee- to-chest place while the leg is kept completely extended on the exam table. If the thigh is elevated off the desk, the test is positive, indicating hip flexor tightness;
- Ely’s test — the patient lies in a prone position, together with the examiner flexing the knee and bringing the heel toward the buttock. If the heel can’t touch the buttocks, then the hip of the side rises from the desk, or the patient feels pain or tingling at the back or thighs, the test is positive suggesting rectus femoris tightness.
In a 2008 study investigated the diagnostic reliability for gluteal tendinopathy of two additional tests: the 30-second single leg stance test and also the resisted external derotation test(5). In the single leg stance test, the individual accounts on one leg for 30 minutes with individual’s hands held by the examiner to limit trunk influence. The test is deemed favorable if pain is experienced at any given time point. From the outside derotation test (see Figure 2), the patient lies in the supine position with the hip flexed to 90 degrees and brought into end range external rotation (or the point of pain). The individual is then asked to return to neutral. Reproduction of pain is considered a positive test.
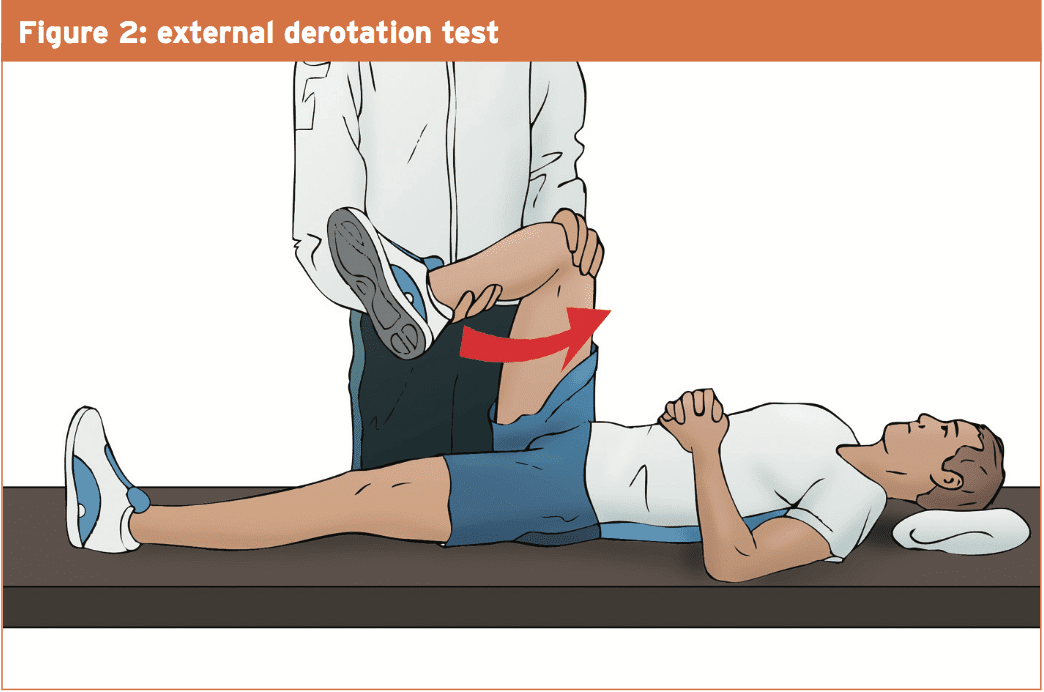 The hip is flexed 90°, and the individual is asked to return the leg into the axis of the table against immunity. When the pain is replicated the test result is positive.
The hip is flexed 90°, and the individual is asked to return the leg into the axis of the table against immunity. When the pain is replicated the test result is positive.
The reliability value of these tests is considered high. In the analysis, two groups of patients were compared with both the evaluations — a target group of 17 patients who were suffering from hip pain anterior, lateral, or posterior to the greater trochanter or involving the thigh, along with a pain-free control group of 19 patients.
In the single-leg, the target group stance reproduced immediate, early, and spontaneous pain in 5 patients, 7, and 5 . The external derotation that was resisted generated pain lying in the supine position. In one of both of these patients, pain has been produced from the position. In the control group, 38 hips were analyzed with only one outcome. Following the tests, MRI imaging was carried, showing tendinopathy and/or bursitis of the gluteus medius and/or minimus tendons.
Statistical analysis showed excellent sensitivity and specificity, with 100 percent and 97.3%, respectively, for its single-leg stance test and 88% and 97.3percent, respectively, for its resisted external derotation test in the supine position. For the latter test, the sensitivity increased to 94% with results that were positive in the prone position in the case of negative effects in the supine position.
Management & Treatment
As with tendinopathies, the main goal is the reduction of pain and dysfunction before progressing to eccentric training. Although no research on the advantages of eccentric training have been carried out especially on gluteal tendinopathy, there’s good evidence in the literature because of this particular rationale, where the therapy of the achilles tendon, patellar tendon, along with lateral epicondylitis are strongly supported(6,7). There are no theoretical reasons why the principles can’t be implemented in the treatment of gluteal tendinopathy.
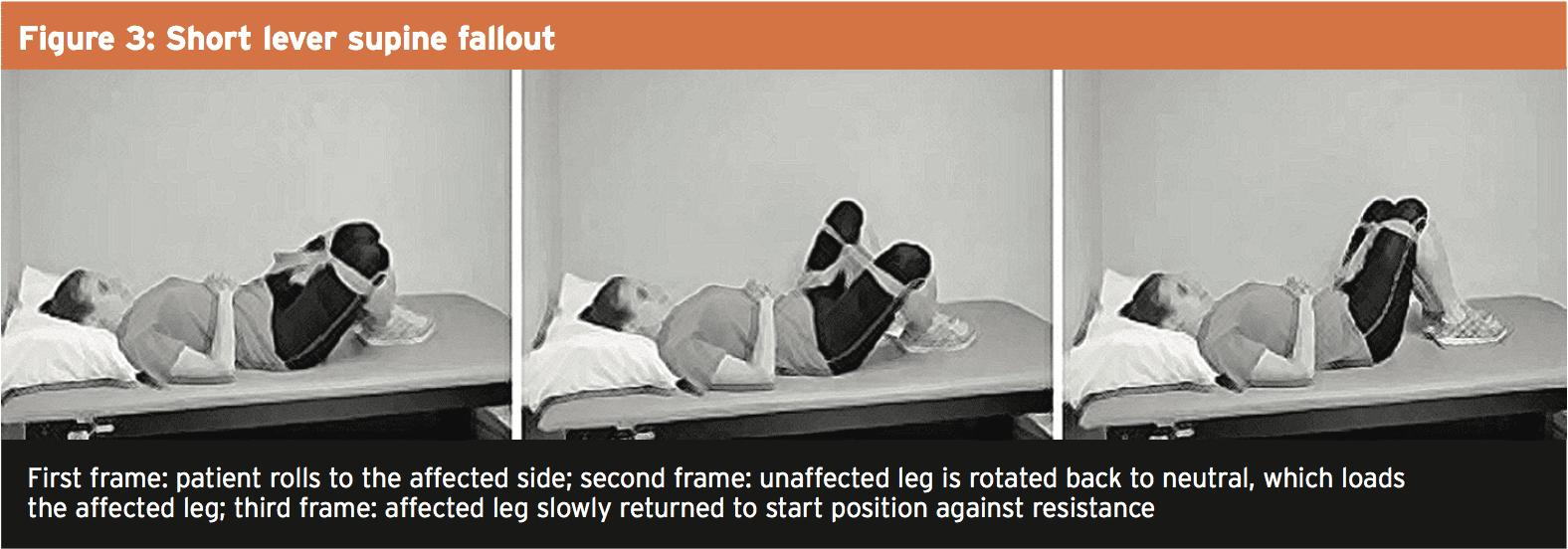
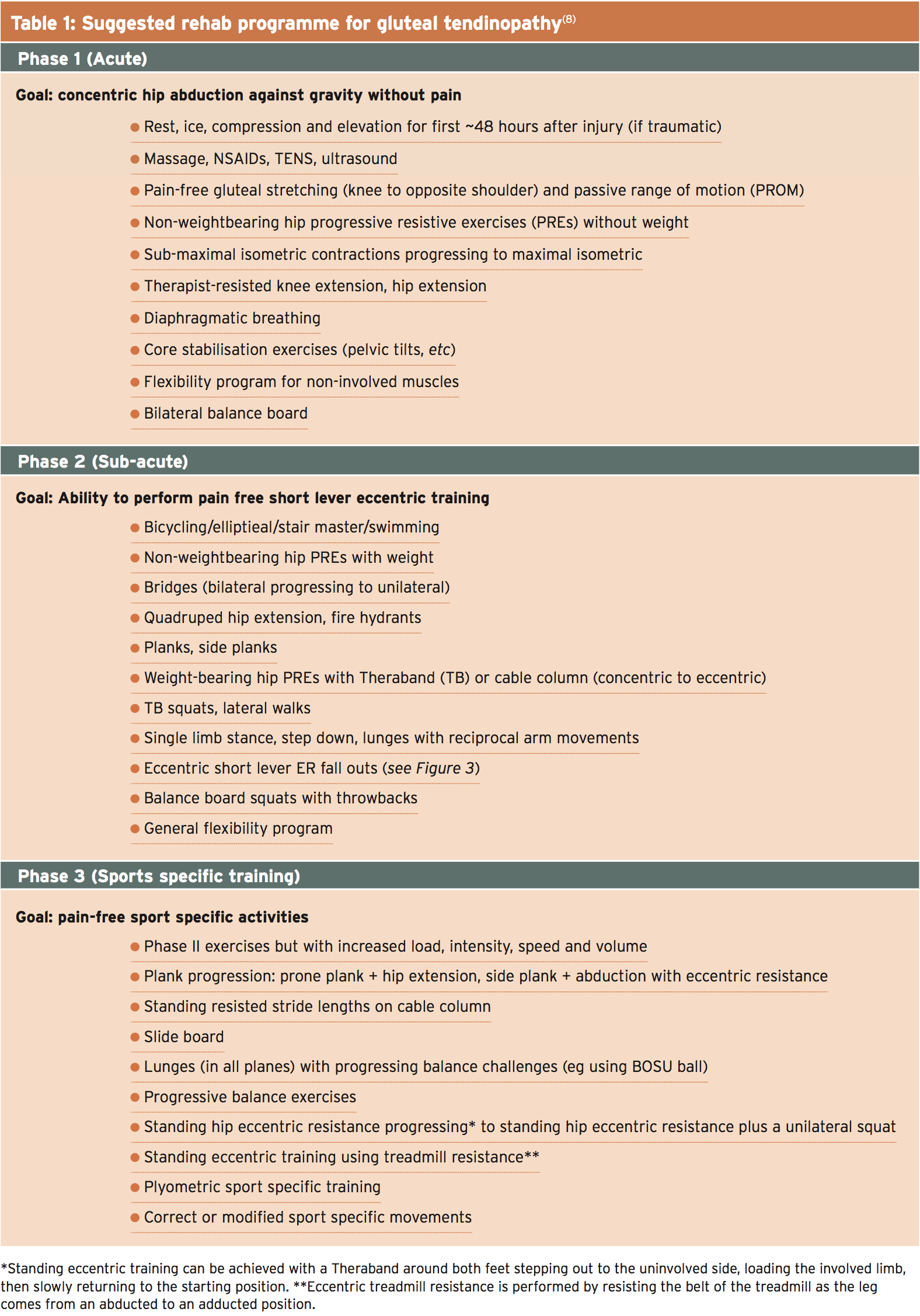 A particularly useful example of training that is gluteal that is bizarre is the ‘short fallout’. Here, the patient rolls towards the affected side then externally rotates the unaffected side, then loading the affected side, and then gradually resists the resistance band to the starting position (see Figure 3). Table 1 shows that a three- stage rehab plan based upon the principles outlined above.
A particularly useful example of training that is gluteal that is bizarre is the ‘short fallout’. Here, the patient rolls towards the affected side then externally rotates the unaffected side, then loading the affected side, and then gradually resists the resistance band to the starting position (see Figure 3). Table 1 shows that a three- stage rehab plan based upon the principles outlined above.
 Overview
Overview
Gluteal tendinopathy is a painful requirement to get an athlete and its diagnosis is not always straightforward. However, a stepwise and comprehensive test in clinic, which includes applicable and tests like the 30-second Single leg stance test and the resisted derotation test will help clinicians arrive at a diagnosis. As with other tendinopathies, that is approached by a rehab focuses on the reduction of pain and dysfunction, followed by a progression to eccentric training that is therapeutic is likely to yield good results.
References
1. Clin J Sport Med. 2011;21(5):447-453
2. Movement, stability and low back pain. New York: Churchill Livingstone; 1997. p.53-71
3. Eur Radiol. 2003; 13: 1339-1347
4. Surg Radiol Anat. 2004; 26: 433-446
5. Arthritis & Rheumatism 2008; 59(2) 241–246
6. Brit J of Sports Med. 2013;47(9):536-544
7. Am J Sports Med. 1998;26(3):360-366
8. Int J Sports Phys Ther. Nov 2014; 9(6): 785–797
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card



 Overview
Overview