Table of Contents
Introduction
The central nervous system consists of the brain and the spinal cord that makes sure that neuron signals are being transmitted all over the body and making sure that it’s working properly. These neuron signals make sure that the gut system, the cardiovascular system, the immune system, and even the endocrine system are working properly and that the neuron signals are being transferred back to the brain with the information. When there are unwanted pathogens that start to attach themselves to the neuron signal, it can cause a disruption to the brain causing neurological disorders to develop over time and wreak havoc on the brain. In this 2 part series, we will be taking a look at what ALS is and how functional neurology diagnoses ALS. Part 1 took a look at what is functional neurology, its relationship with functional medicine, and how functional neurology can help dampen the effects of neurological disorders. By referring patients to qualified and skilled providers who specialized in neurological services. To that end, and when appropriate, we advise our patients to refer to our associated medical providers based on their examination. We find that education is the key to asking valuable questions to our providers. Dr. Alex Jimenez DC provides this information as an educational service only. Disclaimer
Can my insurance cover it? Yes, in case you are uncertain here is the link to all the insurance providers we cover. If you have any questions, please call Dr. Jimenez at 915-850-0900.
What Is ALS?
ALS(Amyotrophic Lateral Sclerosis) or as it is commonly known as “Lou Gehrig’s” disease is a progressive nervous system disease that affects the nerve cells in both the brain and spinal cord, as research shows. Since amyotrophic come from Greece, it means that there is “no muscle nourishment” while lateral identifies the area of the spinal cord where portions of the nerve cells that signal and control muscles, called motor neurons are located and sclerosis refers to scarring or hardening in the region of the lateral spinal cord.
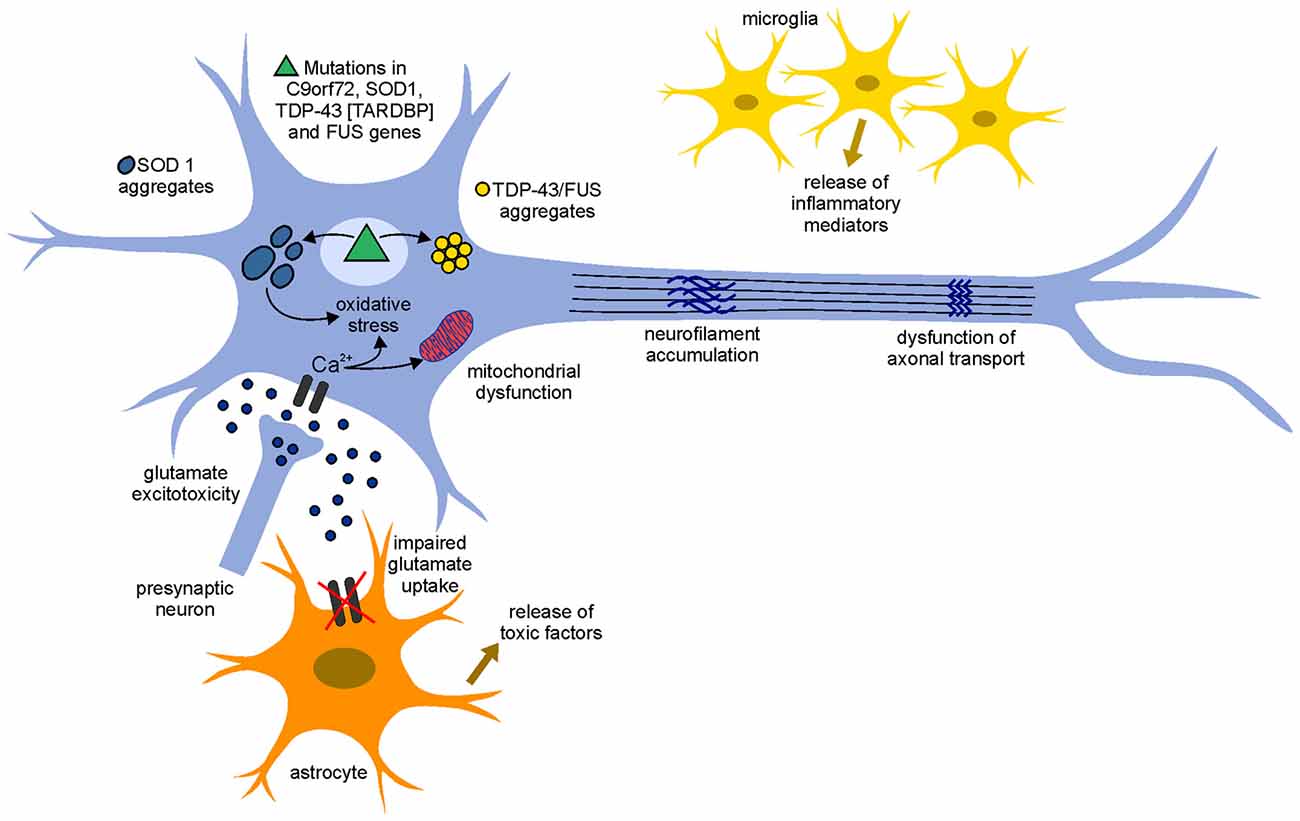
By putting the entire words together, ALS means that there is no nourishment to the motor neurons that are located in the spinal cord. Research also shows that ALS actually belongs to a wide group known as motor neuron diseases that causes gradual degeneration and eventually death to the motor neuron signals and over time cause the brain to lose the ability to control voluntary movements to the body.
The Symptoms
Research has found that ALS affects both the upper and lower motor neurons causing them to decline gradually until they can’t send signals to the muscles. The lower limbs will begin to cause a person to trip, stumble, make them feel really awkward when they are running. When this happens to the lower limbs, the foot will drop or cause a slapping gait. While the upper limbs will cause reduced finger dexterity, cramping, stiffness, and weakness of the intrinsic hand muscles. This will cause a person to have difficulty doing everyday tasks like buttoning clothes, picking up small objects, or turning a key. Other symptoms that ALS causes on the body include:
- Muscle weakness
- Difficulty with speech and swallowing
- Unsteadiness
- Spastic tone
- Brisk or depressed deep tendon reflexes (maybe a mixture of both)
- Muscle atrophy
- Fasciculations
ALS & Cell Death
So caspases are a family of protein‐cutting enzymes that plays a key role in apoptosis, which is the removal of unwanted or damaged cells. Studies have shown that apoptosis occurs naturally and is normal during the development, aging, and homeostatic mechanism to maintain the body’s cellular population in the muscle tissue. Apoptosis is also a defense mechanism for the immune system when cells are being damaged by diseases or toxins. When apoptosis is activated, caspases initiate “death” programs (apoptosis) by destroying key components of the cellular infrastructure and activating factors that mediate damage to the cells. The caspases then let the upstream initiators (activated by the cell‐death signal, e.g., TNF‐alpha) and downstream executioners (directly mediate the events that lead to the demise of the cell). Once that is done, then the executioner caspases activate the machinery that degrades DNA – one example is caspase‐3.
HCTP Therapy
Stem cells* or HCTP (human cellular tissue products) have been used in affiliated clinics and distribution organizations (both international and national) in regenerative cellular treatment. What HCTP does is that it helps boost the body’s own natural healing process by regenerating and repairing damaged cells, diseased organs, and tissues back to their original state and function. With more and upcoming research on the beneficial uses of HCTP, many individuals will begin to feel pain-free and continue on their wellness journey.
Functional Neurology & ALS
In part 1, it discussed what functional neurology is and how it is used to diagnose many neurological disorders that are affecting the brain and the body. Since ALS is a progressive neurodegenerative disease that causes muscle failure, research shows that the use of functional neurology can provide both the patients and medical professionals many opportunities to improve the diagnosis and even establish candidate biomarkers for future therapeutic strategies to dampen the progression of ALS.
Nutrition & ALS
When individuals are suffering from ALS, research shows that ALS increases the high risk of malnutrition causing symptoms of dysphagia, depression, cognitive impairment, difficulty with self‐feeding and meal preparation, hypermetabolism, anxiety, respiratory insufficiency, and fatigue with meals to individuals. However, incorporating nutritional foods that are higher in antioxidants and fiber‐rich foods such as fruit and vegetables can reduce the risk of ALS. Even consuming foods high in ω‐3 PUFAs may help prevent or delay the onset of ALS.
Exercise & ALS
Moderate exercise has been shown to improve strength and prolong survival in animal models of ALS and should not be avoided. Studies have found that proper exercise is highly important for preventing atrophy of the muscles, particularly in the early stages of ALS. Sedentary behavior leads to deconditioning and weakness caused by the disease itself, thus contributing to muscle and joint tightness, contractures, and pain. Some of the benefits of moderate exercise can help increase appetite, digestion, mood, sleep, positive impact on hormones/trophic factors (including BDNF and IGF‐1), and inflammatory markers. However, if a person has fatigue or pain that lasts longer than 30 minutes after exercise, the program needs to be reduced and modified but still, give beneficial results.
Conclusion
All in all, ALS is a progressive neurological disease that causes muscle failure in the body. By utilizing functional neurology and creating a treatment plan on dampening the progressive effects, many individuals can be pain-free and feel great. Even though ALS is chronic and there is no cure yet, by making small changes in the food a person eats and incorporating moderate exercises, the body has a chance to live longer.
References
de Almeida, J P Lopes, et al. “Exercise and Amyotrophic Lateral Sclerosis.” Neurological Sciences: Official Journal of the Italian Neurological Society and of the Italian Society of Clinical Neurophysiology, U.S. National Library of Medicine, Feb. 2012, https://pubmed.ncbi.nlm.nih.gov/22228269/.
Dharmadasa, Thanuja, et al. “Implications of Structural and Functional Brain Changes in Amyotrophic Lateral Sclerosis.” Expert Review of Neurotherapeutics, U.S. National Library of Medicine, 19 Apr. 2018, https://pubmed.ncbi.nlm.nih.gov/29667443/.
Elmore, Susan. “Apoptosis: A Review of Programmed Cell Death.” Toxicologic Pathology, U.S. National Library of Medicine, June 2007, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2117903/.
Medical Professional, NINDS. “Amyotrophic Lateral Sclerosis (ALS) Fact Sheet.” National Institute of Neurological Disorders and Stroke, U.S. Department of Health and Human Services, 26 Apr. 2021, https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Amyotrophic-Lateral-Sclerosis-ALS-Fact-Sheet.
Medical Professionals, Cleveland Clinic. “Amyotrophic Lateral Sclerosis: What Is It, Symptoms & Management.” Cleveland Clinic, 15 June 2021, https://my.clevelandclinic.org/health/diseases/16729-amyotrophic-lateral-sclerosis-als.
Nieves, Jeri W, et al. “Association between Dietary Intake and Function in Amyotrophic Lateral Sclerosis.” JAMA Neurology, U.S. National Library of Medicine, 1 Dec. 2016, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5370581/.
Staff, Mayo Clinic. “Amyotrophic Lateral Sclerosis (ALS).” Mayo Clinic, Mayo Foundation for Medical Education and Research, 22 Feb. 2022, https://www.mayoclinic.org/diseases-conditions/amyotrophic-lateral-sclerosis/symptoms-causes/syc-20354022.
Disclaimer
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card





Comments are closed.