Treating Chronic Tension Headaches: What You Need to Know
For individuals affected by headaches that occur 15 or more days a month for more than three months, can knowing the signs and symptoms help healthcare providers help treat and prevent chronic tension headaches?
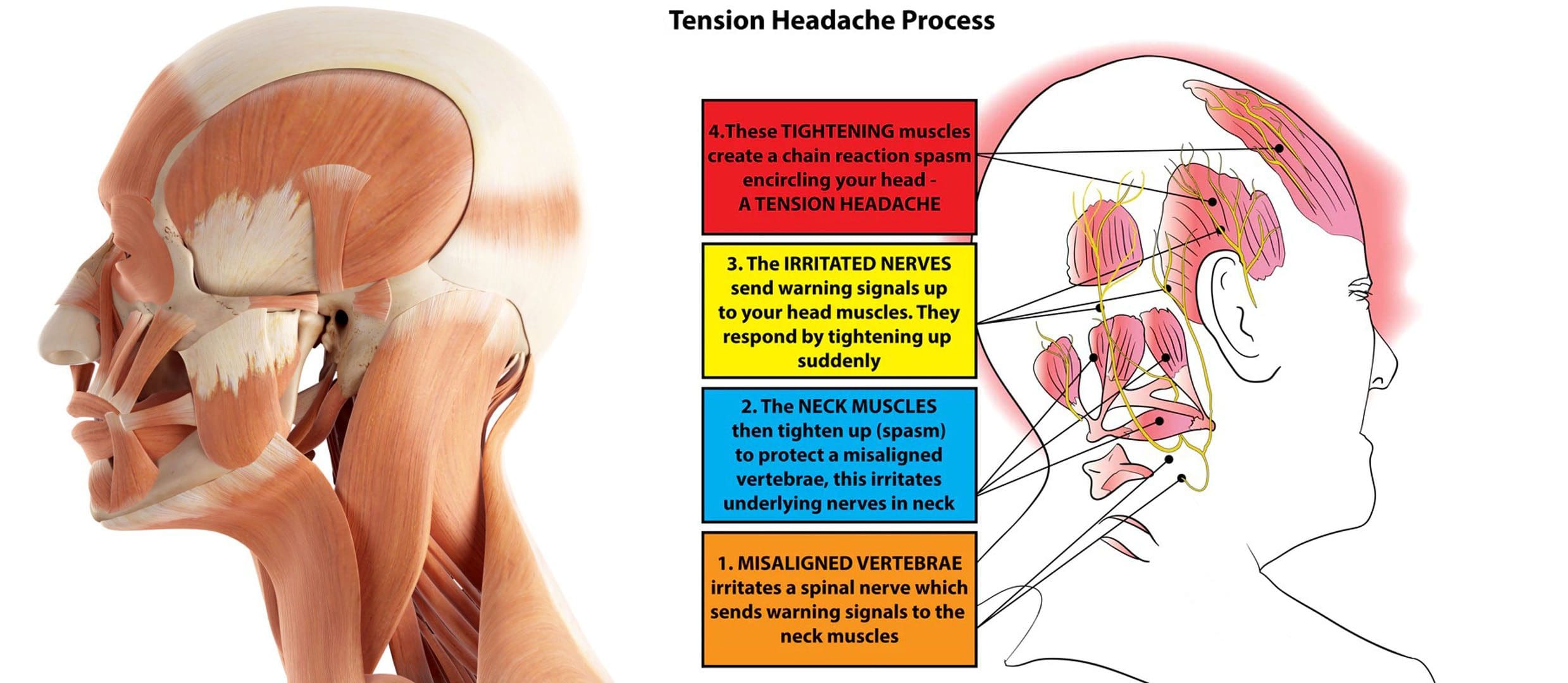
Table of Contents
Chronic Tension Headaches
Most individuals have experienced a tension-type headache. The pain is usually described as a dull tightening or pressure on both sides of the head, like having a tightening band around the head. Some individuals experience these headaches frequently, a condition known as chronic tension headaches. Chronic tension headaches are uncommon but can be debilitating, as they can interfere with a healthy quality of life and daily living.
- Tension headaches are typically caused by stress, anxiety, dehydration, fasting, or lack of sleep and usually resolve with over-the-counter medications. (Cleveland Clinic. 2023)
- This is a primary headache disorder that affects around 3% of the population.
- Chronic tension headaches can occur daily and negatively impact the quality of life and daily functioning. (Cleveland Clinic. 2023)
Symptoms
- Tension headaches can be referred to as stress headaches or muscle contraction headaches.
- They can present with dull, aching pain and include tightness or pressure across the forehead, sides, or back of the head. (Cleveland Clinic. 2023)
- Additionally, some individuals experience tenderness on the scalp, neck, and shoulders.
- Chronic tension headaches materialize 15 or more days a month on average for more than three months.
- The headache can last for several hours or be continuous for several days.
Causes
- Tension headaches are typically caused by tight muscles in the shoulders, neck, jaw, and scalp.
- Teeth grinding/bruxism and jaw clenching can also contribute to the condition.
- Headaches can be brought on by stress, depression, or anxiety and are more common in individuals who:
- Work long hours in stressful jobs.
- Don’t get enough sleep.
- Skip meals.
- Frequently consume alcohol. (Cleveland Clinic. 2023)
Diagnosis
Individuals experiencing headaches that interfere with daily life or need to take medication more than twice a week are recommended to consult a healthcare provider. Before the appointment, it can be helpful to keep a headache diary:
- Record the days
- Times
- Description of the pain, intensity, and other symptoms.
Some questions the healthcare provider may ask include:
- Is the pain pulsating, sharp, or stabbing, or is it constant and dull?
- Where is the pain most intense?
- Is it all over the head, on one side, on the forehead, or behind the eyes?
- Do the headaches interfere with sleep?
- Is working or doing tasks difficult or impossible?
A healthcare provider will likely be able to diagnose the condition based on symptoms alone. However, if the headache pattern is unique or different, the provider may order imaging tests, like MRI or CT scans, to rule out other diagnoses. Chronic tension headaches can be confused with other chronic daily headache disorders like chronic migraine, hemicrania continua, temporomandibular joint dysfunction/TMJ, or cluster headaches. (Fayyaz Ahmed. 2012)
Treatment
Pharmacological therapy for chronic tension headaches usually involves preventive medication.
- Amitriptyline is one medication that has been found to be beneficial in chronic tension headache prevention.
- A tricyclic antidepressant is a sedating medication and is usually taken before sleeping. (Jeffrey L. Jackson et al., 2017)
- According to a meta-analysis of 22 published studies in the Journal of General Internal Medicine, these medications are superior to placebo in reducing headache frequency, with an average of 4.8 fewer headache days per month.
Additional preventive medications may include other antidepressants like:
- Remeron – mirtazapine.
- Anti-seizure medications – like Neurontin – gabapentin, or Topamax – topiramate.
A healthcare provider may also prescribe medication to treat headache episodes, which include:
- Prescription non-steroidal anti-inflammatory drugs or NSAIDs, including acetaminophen, naproxen, indomethacin, or ketorolac.
- Opiates
- Muscle relaxants
- Benzodiazepines – Valium
Non-Medication Treatment
Behavioral therapies are sometimes used on their own or in combination with medication to prevent and manage chronic tension headaches. Examples include:
Acupuncture
- An alternative therapy that involves using needles to stimulate specific points on the body believed to connect with certain pathways/meridians that carry vital energy/chi throughout the body.
Biofeedback
- In Electromyography – EMG biofeedback, electrodes are placed on the scalp, neck, and upper body to detect muscle contraction.
- The patient is trained to control muscle tension to prevent headaches. (William J. Mullally et al., 2009)
- The process can be costly and time-consuming, and there is little evidence to support its effectiveness.
Physical Therapy
- A physical therapist can work out stiff and tight muscles.
- Train individuals on stretches and targeted exercises for loosening tight head and neck muscles.
Cognitive Behavioral Therapy/CBT
- Involves learning how to identify headache triggers and cope in a less stressful and more adaptive way.
- Headache specialists often recommend CBT in addition to medication when developing a treatment plan. (Katrin Probyn et al., 2017)
- Teeth-grinding and jaw-clenching training/treatment can help when they are contributors.
- Regular exercise, as well as practicing healthy sleep hygiene, can be beneficial in prevention.
Supplements
Some individuals with chronic tension headaches may find relief using supplements. The American Academy of Neurology and the American Headache Society report the following supplements can be effective: (National Center for Complementary and Integrative Health. 2021)
- Butterbur
- Feverfew
- Magnesium
- Riboflavin
If the headaches come on suddenly, cause waking up from sleep, or last for days, it’s important to consult a healthcare provider to rule out any underlying causes and develop a personalized treatment plan.
Tension Headaches
References
Cleveland Clinic. (2023). Tension Headaches.
Ahmed F. (2012). Headache disorders: differentiating and managing the common subtypes. British journal of pain, 6(3), 124–132. https://doi.org/10.1177/2049463712459691
Jackson, J. L., Mancuso, J. M., Nickoloff, S., Bernstein, R., & Kay, C. (2017). Tricyclic and Tetracyclic Antidepressants for the Prevention of Frequent Episodic or Chronic Tension-Type Headache in Adults: A Systematic Review and Meta-Analysis. Journal of general internal medicine, 32(12), 1351–1358. https://doi.org/10.1007/s11606-017-4121-z
Mullally, W. J., Hall, K., & Goldstein, R. (2009). Efficacy of biofeedback in the treatment of migraine and tension type headaches. Pain physician, 12(6), 1005–1011.
Probyn, K., Bowers, H., Mistry, D., Caldwell, F., Underwood, M., Patel, S., Sandhu, H. K., Matharu, M., Pincus, T., & CHESS team. (2017). Non-pharmacological self-management for people living with migraine or tension-type headache: a systematic review including analysis of intervention components. BMJ open, 7(8), e016670. https://doi.org/10.1136/bmjopen-2017-016670
National Center for Complementary and Integrative Health. (2021). Headaches: What You Need To Know.
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card



Comments are closed.