Concussions are traumatic brain injuries that affect brain function. Effects from these injuries are often temporary but can include headaches, problems with concentration, memory, balance and coordination. Concussions are usually caused by a blow to the head or violent shaking of the head and upper body. Some concussions cause loss of consciousness, but most do not. And it is possible to have a concussion and not realize it. Concussions are common in contact sports, such as football. However, most people gain a full recovery after a concussion.
Table of Contents
Concussions
Traumatic Brain Injuries (TBI)
- Most often the result of head trauma
- Can also happen due to excessive shaking of the head or acceleration/deceleration
- Mild injuries (mTBI/concussions) are the most common type of brain injury
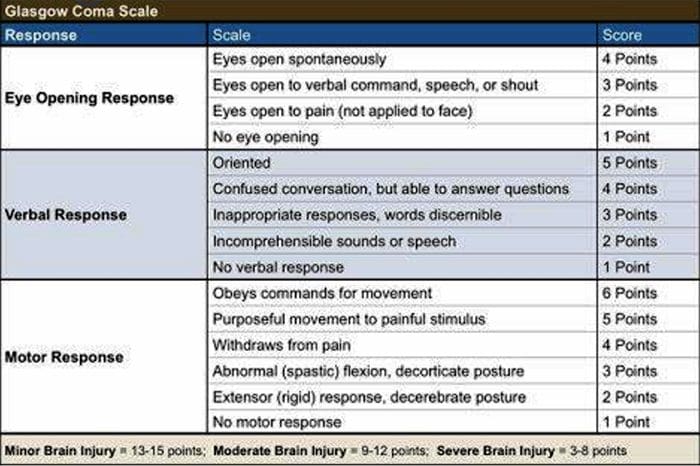
Glasgow Coma Scale
Common Causes Of Concussion
- Motor vehicle collisions
- Falls
- Sports injuries
- Assault
- Accidental or intentional discharge of weapons
- Impact with objects
Prevention
Prevention of concussive injuries can be paramount
Encourage Patients To Wear Helmets
- Competitive sports, especially boxing, hokey, football and baseball
- Horseback riding
- Riding bicycles, motorcycles, ATVs, etc.
- High elevation activates such as rock climbing, zip lining
- Skiing, snowboarding
Encourage Patients To Wear Seatbelts
- Discuss the importance of wearing seatbelts at all times in vehicles with all of your patients
- Also encourage use of appropriate booster or car seats for children to ensure adequate fit and function of seat belts.
Driving Safely
- Patients should never drive while under the influence of drugs, including certain medications or alcohol
- Never text and drive
Make Spaces Safer For Children
- Install baby gates and window latches in the home
- May in areas with shock-absorbing material, such as hardwood mulch or sand
- Supervise children carefully, especially when they’re near water
Prevent Falls
- Clearing tripping hazards such as loose rugs, uneven flooring or walkway clutter
- Using nonslip mats in the bathtub and on shower floors, and installing grab bars next to the toilet, tub and shower
- Ensure appropriate footwear
- Installing handrails on both sides of stairways
- Improving lighting throughout the home
- Balance training exercises
Balance Training
- Single leg balance
- Bosu ball training
- Core strengthening
- Brain balancing exercises
Concussion Verbiage
Concussion vs. mTBI (mild traumatic brain injury)
- mTBI is the term being used more commonly in medical settings, but concussion is a more largely recognized term in the community by sports coaches, etc.
- The two terms describe the same basic thing, mTBI is a better term to use in your charting
Evaluating Concussion
- Remember that there does not always have to be loss of consciousness for there to be a concussion
- Post-Concussion Syndrome can occur without LOC as well
- Symptoms of concussion may not be immediate and could take days to develop
- Monitor for 48 post head injury watching for red flags
- Use Acute concussion evaluation (ACE) form to gather information
- Order imaging (CT/MRI) as needed if concussion red flags are present
Red Flags
Requires imaging (CT/MRI)
- Headaches worsening
- Patient appears drowsy or can’t be awakened
- Has difficulty recognizing people or places
- Neck pain
- Seizure activity
- Repeated vomiting
- Increasing confusion or irritability
- Unusual behavioral change
- Focal neurologic signs
- Slurred speech
- Weakness or numbness in extremities
- Change in state of consciousness
Common Symptoms Of Concussion
- Headache or a sensation of pressure in the head
- Loss of or alteration of consciousness
- Blurred eyesight or other vision problems, such as dilated or uneven pupils
- Confusion
- Dizziness
- Ringing in the ears
- Nausea or vomiting
- Slurred speech
- Delayed response to questions
- Memory loss
- Fatigue
- Trouble concentrating
- Continued or persistent memory loss
- Irritability and other personality changes
- Sensitivity to light and noise
- Sleep problems
- Mood swings, stress, anxiety or depression
- Disorders of taste and smell
Mental/Behavioral Changes
- Verbal outbursts
- Physical outbursts
- Poor judgment
- Impulsive behavior
- Negativity
- Intolerance
- Apathy
- Egocentricity
- Rigidity and inflexibility
- Risky behavior
- Lack of empathy
- Lack of motivation or initiative
- Depression or anxiety
Symptoms In Children
- Concussions can present differently in children
- Excessive crying
- Loss of appetite
- Loss of interest in favorite toys or activities
- Sleep issues
- Vomiting
- Irritability
- Unsteadiness while standing
Amnesia
Memory loss and failure to form new memories
Retrograde Amnesia
- Inability to remember things that happened before the injury
- Due to failure in recall
Anterograde Amnesia
- Inability to remember things that happened after the injury
- Due to failure to formulate new memories
Even short memory losses can be predictive of outcome
- Amnesia may be up to 4-10 times more predictive of symptoms and cognitive deficits following concussion than is LOC (less than 1 minute)
Return To Play Progression
Baseline: No Symptoms
- As the baseline step of the Return to Play Progression, the athlete needs to have completed physical and cognitive rest and not be experiencing concussion symptoms for a minimum of 48 hours. Keep in mind, the younger the athlete, the more conservative the treatment.
Step 1: Light Aerobic Activity
- The Goal: Only to increase an athlete’s heart rate.
- The Time: 5 to 10 minutes.
- The Activities: Exercise bike, walking, or light jogging.
- Absolutely no weight lifting, jumping or hard running.
Step 2: Moderate activity
- The Goal: Limited body and head movement.
- The Time: Reduced from typical routine.
- The Activities: Moderate jogging, brief running, moderate-intensity stationary biking, and moderate-intensity weightlifting
Step 3: Heavy, non-contact activity
- The Goal: More intense but non-contact
- The Time: Close to typical routine
- The Activities: Running, high-intensity stationary biking, the player’s regular weightlifting routine, and non- contact sport-specific drills. This stage may add some cognitive component to practice in addition to the aerobic and movement components introduced in Steps 1 and 2.
Step 4: Practice & full contact
- The Goal: Reintegrate in full contact practice.
Step 5: Competition
- The Goal: Return to competition.
Microglial Priming
After head trauma microglial cells are primed and can become over active
- To combat this, you must mediate the inflammation cascade
Prevent repeated head trauma
- Due to priming of the foam cells, response to follow-up trauma may be far more severe and damaging
What Is Post-Concussion Syndrome (PCS)?
- Symptoms following head trauma or mild traumatic brain injury, that can last weeks, months or years after injury
- Symptoms persist longer than expected after initial concussion
- More common in women and persons of advanced age who suffer head trauma
- Severity of PCS often does not correlate to severity of head injury
PCS Symptoms
- Headaches
- Dizziness
- Fatigue
- Irritability
- Anxiety
- Insomnia
- Loss of concentration and memory
- Ringing in the ears
- Blurry vision
- Noise and light sensitivity
- Rarely, decreases in taste and smell
Concussion Associated Risk Factors
- Early symptoms of headache after injury
- Mental changes such as amnesia or fogginess
- Fatigue
- Prior history of headaches
Evaluation Of PCS
PCS is a diagnosis of exclusion
- If patient presents with symptoms after head injury, and other possible causes have been ruled out => PCS
- Use appropriate testing and imaging studies to rule out other causes of symptoms
Headaches In PCS
Often “tension” type headache
Treat as you would for tension headache
- Reduce stress
- Improve stress coping skills
- MSK treatment of the cervical and thoracic regions
- Constitutional hydrotherapy
- Adrenal supportive/adaptogenic herbs
Can be migraine, especially in people who had pre-existing migraine conditions prior to injury
- Reduce inflammatory load
- Consider management with supplements and or medications
- Reduce light and sound exposure if there is sensitivity
Dizziness In PCS
- After head trauma, always assess for BPPV, as this is the most common type of vertigo after trauma
- Dix-Hallpike maneuver to diagnose
- Epley’s maneuver for treatment
Light & Sound Sensitivity
Hypersensitivity to light and sound is common in PCS and typically exacerbates other symptoms such as headache and anxiety
Management of excess mesencephalon stimulation is crucial in such cases
- Sunglasses
- Other light blocking glasses
- Earplugs
- Cotton in ears
Treatment Of PCS
Manage each symptom individually as you otherwise would
Manage CNS inflammation
- Curcumin
- Boswelia
- Fish oil/Omega-3s – (***after r/o bleed)
Cognitive behavioral therapy
- Mindfulness & relaxation training
- Acupuncture
- Brain balancing physical therapy exercises
- Refer for psychological evaluation/treatment
- Refer to mTBI specialist
mTBI Specialists
- mTBI is difficult to treat and is an entire specialty both in the allopathic and complementary medicine
- Primary objective is to recognize and refer for appropriate care
- Pursue training in mTBI or plan to refer to TBI specialists
Sources
- “A Head for the Future.” DVBIC, 4 Apr. 2017, dvbic.dcoe.mil/aheadforthefuture.
- Alexander G. Reeves, A. & Swenson, R. Disorders of the Nervous System. Dartmouth, 2004.
- “Heads Up to Health Care Providers.” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, 16 Feb. 2015, www.cdc.gov/headsup/providers/.
- “Post-Concussion Syndrome.” Mayo Clinic, Mayo Foundation for Medical Education and Research, 28 July 2017, www.mayoclinic.org/diseases-conditions/post- concussion-syndrome/symptoms-causes/syc-20353352.
Post Disclaimer
Professional Scope of Practice *
The information herein on "Concussions & Post-Concussion Syndrome" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Our information scope is limited to Chiropractic, musculoskeletal, physical medicines, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somatovisceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and/or functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.*
Our office has reasonably attempted to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez, DC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, RN*, CCST, IFMCP*, CIFM*, ATN*
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807, New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Florida
Florida License RN License # RN9617241 (Control No. 3558029)
License Compact Status: Multi-State License: Authorized to Practice in 40 States*
Presently Matriculated: ICHS: MSN* FNP (Family Nurse Practitioner Program)
Dr. Alex Jimenez DC, MSACP, RN* CIFM*, IFMCP*, ATN*, CCST
My Digital Business Card