[et_pb_section bb_built=”1″][et_pb_row][et_pb_column type=”4_4″][et_pb_text]
Neurodegenerative disorders are on the rise worldwide. In the USA alone nearly 5.4 million individuals suffer from Alzheimer’s disease, while roughly 500,000 suffer from Parkinson’s disease. As the American population ages, these numbers are just likely to increase. A large proportion of individuals have direct experience with neurodegenerative disorders either on their own or through their loved ones. Brain disorders like Parkinson’s, Huntington’s or Alzheimer’s, have some of the maximum disease burdens.
Illness burden, according to the World Health Organization, or WHO, characterizes the amount of healthy years that are influenced by disability. Neurodegenerative disorders are more burdensome because they not only affect the person, but also have an enormous financial, emotional and physical effect on households. The disease burden for neurodegenerative disorders has been calculated to be more significant than that of cancers. As scientific research expands into the realm of medical marijuana, and its various beneficial elements, there’s beginning to be significant excitement surrounding the treatment possibilities for neurodegenerative ailments with CBD, or cannabidiol, oil.
Research studies into CBD for neurodegenerative diseases, including Huntington’s, Parkinson’s and Alzheimer’s, appears to be overwhelmingly positive. Not only does CBD, or cannabidiol, treatment target some of the most painful symptoms of these diseases but CBD also seems to indicate little to no side effect risk. For a lot of people managing their symptoms, CBD is offering a ray of hope for an assortment of progressively severe neurological diseases. The purpose of the following article is to demonstrate as well as discuss the effects of cannabidiol for the treatment and prevention of neurodegenerative disorders.
Table of Contents
Cannabidiol for Neurodegenerative Disorders: Important New Clinical Applications for this Phytocannabinoid?
Abstract
Cannabidiol (CBD) is a phytocannabinoid with therapeutic properties for numerous disorders exerted through molecular mechanisms that are yet to be completely identified. CBD acts in some experimental models as an anti-inflammatory, anticonvulsant, anti-oxidant, anti-emetic, anxiolytic and antipsychotic agent, and is therefore a potential medicine for the treatment of neuroinflammation, epilepsy, oxidative injury, vomiting and nausea, anxiety and schizophrenia, respectively. The neuroprotective potential of CBD, based on the combination of its anti-inflammatory and anti-oxidant properties, is of particular interest and is presently under intense preclinical research in numerous neurodegenerative disorders. In fact, CBD combined with Δ9-tetrahydrocannabinol is already under clinical evaluation in patients with Huntington’s disease to determine its potential as a disease-modifying therapy. The neuroprotective properties of CBD do not appear to be exerted by the activation of key targets within the endocannabinoid system for plant-derived cannabinoids like Δ9-tetrahydrocannabinol, i.e. CB1 and CB2 receptors, as CBD has negligible activity at these cannabinoid receptors, although certain activity at the CB2 receptor has been documented in specific pathological conditions (i.e. damage of immature brain). Within the endocannabinoid system, CBD has been shown to have an inhibitory effect on the inactivation of endocannabinoids (i.e. inhibition of FAAH enzyme), thereby enhancing the action of these endogenous molecules on cannabinoid receptors, which is also noted in certain pathological conditions. CBD acts not only through the endocannabinoid system, but also causes direct or indirect activation of metabotropic receptors for serotonin or adenosine, and can target nuclear receptors of the PPAR family and also ion channels.
Keywords: cannabidiol, cannabinoid signalling system, Huntington’s disease, neonatal ischaemia, neuroprotection, Parkinson’s disease
Overview on the Therapeutic Properties of CBD
Cannabidiol (CBD) is one of the key cannabinoid constituents in the plant Cannabis sativa in which it may represent up to 40% of cannabis extracts [1]. However, contrarily to Δ9-tetrahydrocannabinol (Δ9-THC), the major psychoactive plant-derived cannabinoid, which combines therapeutic properties with some important adverse effects, CBD is not psychoactive (it does not activate CB1 receptors [2]), it is well-tolerated and exhibits a broad spectrum of therapeutic properties [3]. Even, combined with Δ9-THC in the cannabis-based medicine Sativex® (GW Pharmaceuticals Ltd, Kent, UK), CBD is able to enhance the beneficial properties of Δ9-THC while reducing its negative effects [4]. Based on this relatively low toxicity, CBD has been studied, even at the clinical level, alone or combined with other phytocannabinoids, to determine its therapeutic efficacy in different central nervous system (CNS) and peripheral disorders [3]. In the CNS, CBD has been reported to have anti-inflammatory properties, thus being useful for neuroinflammatory disorders [5], including multiple sclerosis for which CBD combined with Δ9-THC (Sativex®) has been recently licenced as a symptom-relieving agent for the treatment of spasticity and pain [6]. Based on its anticonvulsant properties, CBD has been proposed for the treatment of epilepsy [7–9], and also for the treatment of sleep disorders based on its capability to induce sleep [10]. CBD is also anti-emetic, as are most of the cannabinoid agonists, but its effects are independent of CB1 receptors and are possibly related to its capability to modulate serotonin transmission (see [11] and below). CBD has antitumoural properties that explain its potential against various types of cancer [12, 13]. Moreover, CBD has recently shown an interesting profile for psychiatric disorders, for example, it may serve as an antipsychotic and be a promising compound for the treatment of schizophrenia [14–17], but it also has potential as an anxiolytic [18] and antidepressant [19], thus being also effective for other psychiatric disorders. Lastly, based on the combination of its anti-inflammatory and anti-oxidant properties, CBD has been demonstrated to have an interesting neuroprotective profile as indicated by results obtained through intense preclinical research into numerous neurodegenerative disorders, in particular the three disorders addressed in this review, neonatal ischaemia (CBD alone) [20], Huntington’s disease (HD) (CBD combined with Δ9-THC as in Sativex®) [21–23] or Parkinson’s disease (PD) (CBD probably combined with the phytocannabinoid Δ9-tetrahydrocannabivarin, Δ9-THCV) [24, 25], work that has recently progressed to the clinical area in some specific cases [26]. The neuroprotective potential of CBD for the management of certain other neurodegenerative disorders, e.g. Alzheimer’s disease, stroke and multiple sclerosis, has also been investigated in studies that have yielded some positive results [27–33]. However, these data will be considered here only very briefly.
Overview on the Mechanisms of Action of CBD
The therapeutic properties of CBD do not appear to be exerted by the activation of key targets within the endocannabinoid system for plant-derived cannabinoids like Δ9-THC, i.e. CB1 and CB2 receptors. CBD has in general negligible activity at these cannabinoid receptors [2], so it has been generally assumed that most of its pharmacological effects are not a priori pharmacodynamic in nature and related to the activation of specific signalling pathways, but related to its innate chemical properties, in particular with the presence of two hydroxyl groups (see below) that enables CBD to have an important anti-oxidant action [2]. However, in certain pathological conditions (i.e. damage of immature brain), CBD has shown some activity at the CB2 receptor exerted directly ([20], see also Table 1) or indirectly through an inhibitory effect on the mechanisms of inactivation (i.e. transporter, FAAH enzyme) of endocannabinoids [34, 35], enhancing the action of these endogenous molecules at the CB2 receptor but also at the CB1 and at other receptors for endocannabinoids, i.e. TRPV1 [35] and TRPV2 [36] receptors.
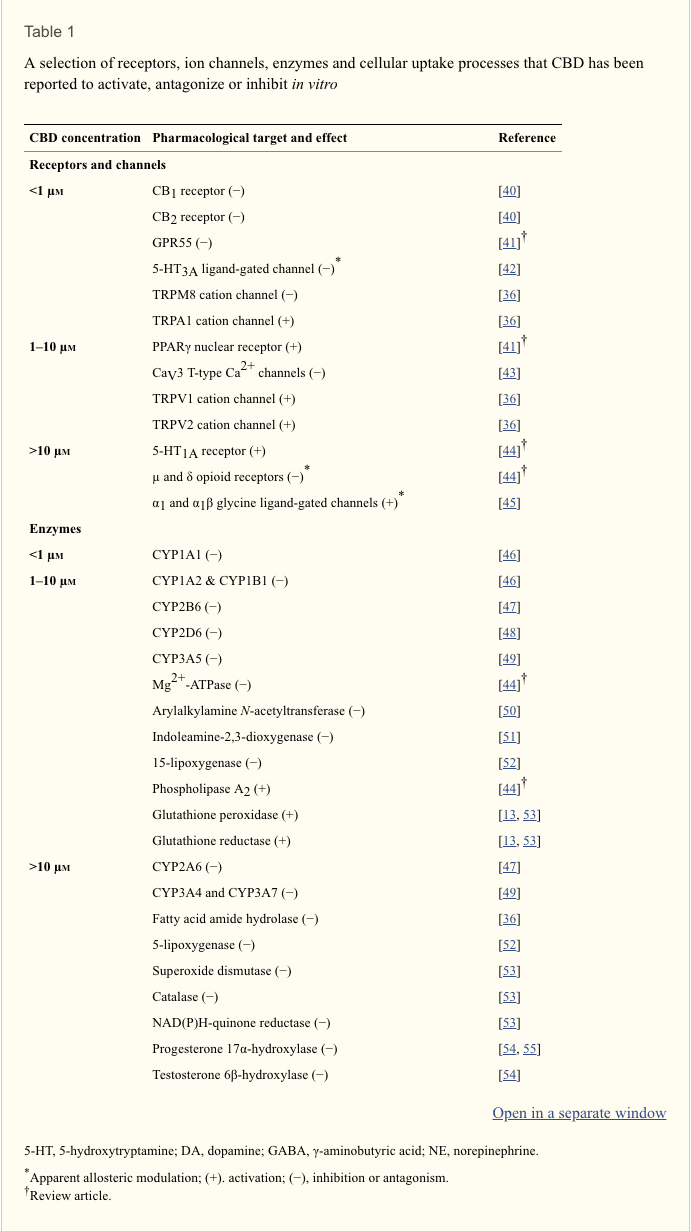
However, the anti-oxidant profile of CBD, as well as the few effects it exerts through targets within the endocannabinoid system in certain pathophysiological conditions, cannot completely explain all of the many pharmacological effects of CBD, prompting a need to seek out possible targets for this phytocannabinoid outside the endocannabinoid system. There is, indeed, already evidence that CBD can affect serotonin receptors (i.e. 5HT1A) [18, 19, 28], adenosine uptake [37], nuclear receptors of the PPAR family (i.e. PPAR-γ) [38, 39] and many other pharmacological targets (see Table 1 including references [40–56]). In part, this information derives from numerous studies directed at identifying the pharmacological actions that CBD produces in vitro. This phytocannabinoid has been found to display a wide range of actions in vitro some at concentrations in the submicromolar range, and others at concentrations between 1 and 10 µm or above 10 µm. Its pharmacological targets include a number of receptors, ion channels, enzymes and cellular uptake processes (summarized in Table 1). There is evidence too that CBD can inhibit delayed rectifier K+ and L-type Ca2+ currents and evoked human neutrophil migration, activate basal microglial cell migration, and increase membrane fluidity, all at submicromolar concentrations, and that at concentrations between 1 and 10 µm it can inhibit the proliferation of human keratinocytes and of certain cancer cells (reviewed in [44]). At concentrations between 1 and 10 µm, CBD has also been reported to be neuroprotective, to reduce signs of oxidative stress, to modulate cytokine release and to increase calcium release from neuronal and glial intracellular stores (reviewed in [44]), and at 15 µM to induce mRNA expression of several phosphatases in prostate and colon cancer cells [57].
As will be discussed in the following section, the question of which of these many actions contributes most towards the beneficial effects that CBD displays in vivo in animal models of neurodegenerative disorders such as PD and HD remains to be fully investigated. Also still to be explored is the possibility that CBD may ameliorate signs and symptoms of such disorders and others (i.e. psychiatric disorders), at least in part, by potentiating activation of 5-HT1A receptors by endogenously released serotonin. Thus, although CBD only activates the 5-HT1A receptor at concentrations above 10 µm (Table 1), it can, at the much lower concentration of 100 nm enhance the ability of the 5-HT1A receptor agonist, 8-hydroxy-2-(di-n-propylamino)tetralin to stimulate [35S]-GTPγS binding to rat brainstem membranes [58]. Furthermore, there is evidence first, that activation of 5-HT1A receptors can ameliorate specific symptoms in PD [59, 60] and second, that beneficial effects displayed by CBD in vivo in animal models of ischaemic injury [27, 28], hepatic encephalopathy [61], anxiety, stress and panic [18, 62–64], depression [19], pain [65] and nausea and vomiting [66] are all mediated by increased activation of the 5-HT1A receptor. Importantly, the dose–response curve of CBD for the production of its effects in several of these models has been found to be bell-shaped [19, 28, 62, 65, 67, 68]. This is a significant observation since it strengthens the hypothesis that CBD can act in vivo to potentiate 5-HT-induced activation of 5-HT1A receptors. Thus, the concentration–response curve of CBD for its enhancement of 8-hydroxy-2-(di-n-propylamino)tetralin-induced stimulation of [35S]-GTPγS binding to rat brainstem membranes is also bell-shaped [58].
CBD as a Neuroprotective Agent
In contrast to the neuroprotective properties of cannabinoid receptor agonists [69, 70], those of CBD do not seem to be attributable to the control of excitotoxicity via the activation of CB1 receptors and/or to the control of microglial toxicity via the activation of CB2 receptors. Thus, except in preclinical models of neonatal ischaemia (see below and [20]), CBD has been found not to display any signs of CB1 or CB2 receptor activation, and yet is no less active than cannabinoid receptor agonists against the brain damage produced by different types of cytotoxic insults ([71–75], reviewed in [76]). What then are the cannabinoid receptor-independent mechanisms by which CBD acts as a neuroprotective agent? Finding the correct answer to this question is not easy, although data obtained in numerous investigations into different pathological conditions associated with brain damage indicate that CBD does normalize glutamate homeostasis [71, 72], reduce oxidative stress [73, 77] and attenuate glial activation and the occurrence of local inflammatory events [74, 78]. Furthermore, a recent study by Juknat et al. [79] has strongly demonstrated the existence of notable differences in the genes that were altered by CBD (not active at CB1 or CB2 receptors) and those altered by Δ9-THC (active at both these receptors) in inflammatory conditions in an in vitro model. These authors found a greater influence of CBD on genes controlled by nuclear factors known to be involved in the regulation of stress responses (including oxidative stress) and inflammation [79]. This agrees with the idea that there may be two key processes underlying the neuroprotective effects of CBD. The first and the most classic mechanism is the capability of CBD to restore the normal balance between oxidative events and anti-oxidant endogenous mechanisms [69] that is frequently disrupted in neurodegenerative disorders, thereby enhancing neuronal survival. As has been mentioned above [73, 77], this capability seems to be inherent to CBD and structurally-similar compounds, i.e. Δ9-THC, cannabinol, nabilone, levonantradol and dexanabinol, as it would depend on the innate anti-oxidant properties of these compounds and be cannabinoid receptor-independent. Alternatively, or in addition, the anti-oxidant effect of CBD may involve intracellular mechanisms that enhance the ability of endogenous anti-oxidant enzymes to control oxidative stress, in particular the signaling triggered by the transcription factor nuclear factor-erythroid 2-related Factor 2 (nrf-2), as has been found in the case of other classic anti-oxidants. According to this idea, CBD may bind to an intracellular target capable of regulating this transcription factor which plays a major role in the control of anti-oxidant-response elements located in genes encoding for different anti-oxidant enzymes of the so-called phase II-anti-oxidant response (see proposed mechanism in Figure 1). This possibility is presently under investigation (reviewed in [69]).
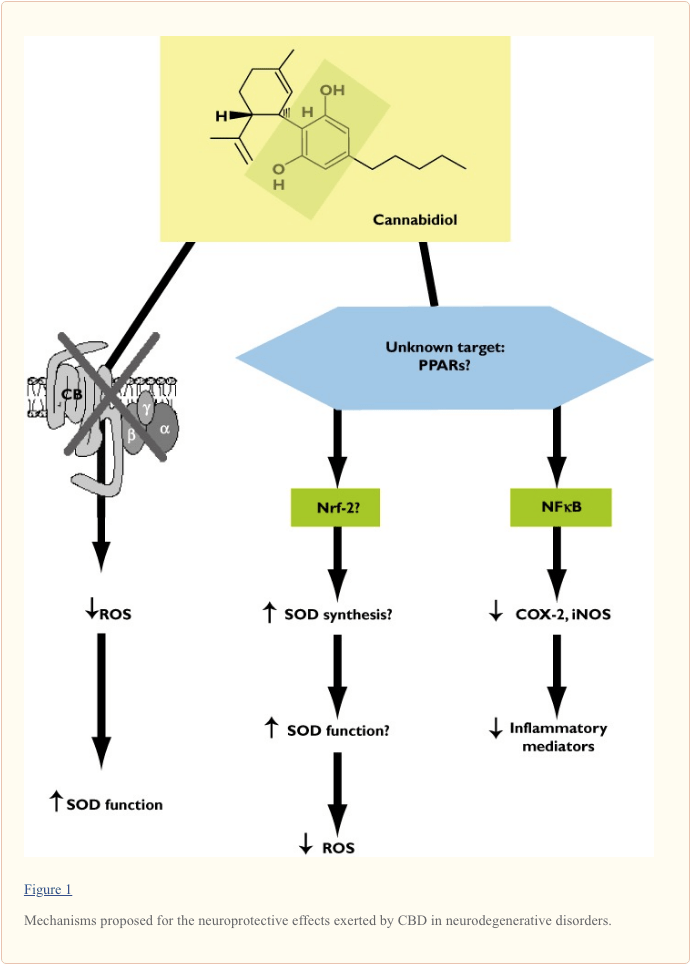
The second key mechanism for CBD as a neuroprotective compound involves its anti-inflammatory activity that is exerted by mechanisms other than the activation of CB2 receptors, the canonic pathway for the anti-inflammatory effects of most of cannabinoid agonists [70]. Anti-inflammatory effects of CBD have been related to the control of microglial cell migration [80] and the toxicity exerted by these cells, i.e. production of pro-inflammatory mediators [81], similarly with the case of cannabinoid compounds targeting the CB2 receptor [70]. However, a key element in this CBD effect is the inhibitory control of NFκB signalling activity and the control of those genes regulated by this transcription factor (i.e. iNOS) [31, 81]. This inhibitory control of NFκB signalling may be exerted by reducing the phosphorylation of specific kinases (i.e. p38 MAP kinase) involved in the control of this transcription factor and by preventing its translocation to the nucleus to induce the expression of pro-inflammatory genes [31]. However, it has been recently proposed that CBD may bind the nuclear receptors of the PPAR family, in particular the PPAR-γ[38, 39] (Table 1) and it is well known that these receptors antagonize the action of NFκB, reducing the expression of pro-inflammatory enzymes (i.e. iNOS, COX-2), pro-inflammatory cytokines and metalloproteases, effects that are elicited by different cannabinoids including CBD (reviewed in [9, 39]). Therefore, it could well be that CBD may produce its anti-inflammatory effects by the activation of these nuclear receptors and the regulation of their downstream signals although various aspects of this mechanism are pending further research and confirmation (see proposed mechanism in Figure 1).
Other mechanisms proposed for the neuroprotective effects of CBD include: (i) the contribution of 5HT1A receptors, e.g. in stroke [27, 28], (ii) the inhibition of adenosine uptake [37], e.g. in neonatal ischaemia ([20], see below) and (iii) specific signalling pathways (e.g. WNT/β-catenin signaling) that play a role in β-amyloid-induced GSK-3β activation and tau hyperphosphorylation in Alzheimer’s disease [82].
CBD in Specific Neurodegenerative Disorders: from Basic to Clinical Studies
Although the neuroprotective properties of CBD have been already examined in numerous acute or chronic neurodegenerative disorders, we will address here only three disorders, i.e. neonatal ischaemia, HD and PD, in which a clinical evaluation of CBD, as monotherapy or in combination with other phytocannabinoids, is already in progress or may be developed soon. CBD has demonstrated significant effects in preclinical models of these three disorders, but, in some cases, its combination with other phytocannabinoids (i.e. Δ9-THC for HD, Δ9-THCV for PD) revealed some interesting synergies that may be extremely useful at the clinical level.
CBD and Neonatal Ischaemia
Brain damage by hypoxia-ischaemia (HI) affects 0.3% subjects over 65 years old in developed countries leading to more than 150 000 deaths per year in the USA (for review see [83]). Although less prevalent, newborn hypoxic-ischaemic brain damage (NHIBD) is of great importance too. Approximately 0.1–0.2% live term births experience perinatal asphyxia with one third of them developing a severe neurological syndrome. About 25% of severe NHIBD leads to lasting sequelae and about 20% to death. Energy failure during ischaemia provokes the dysfunction of ionic pumps in neurons, leading to accumulation of ions and excitotoxic substances such as glutamate. The consequent increase in intracellular calcium content aggravates the neuron dysfunction and activates different enzymes, starting different processes of immediate and programmed cell death. During post ischaemic reperfusion, inflammation and oxidative stress aggravate and amplify such responses, increasing and spreading neuron and glial cell damage. Excitotoxicity, inflammation and oxidative stress play, therefore, a particularly relevant role in HI-induced brain cell death in newborns [83].
Unfortunately, the therapeutic outcome in NHIBD is still very limited and there is a strong need for novel strategies. We have solid evidence that CBD may be a good candidate to be tested in NHIBD at the clinical level. Using forebrain slices from newborn mice subjected to glucose-oxygen deprivation, a well-known in vitro model of NHIBD, we have already reported that CBD is able to reduce necrotic and apoptotic damage [20]. This neuroprotective effect is related to the modulation of excitotoxicity, oxidative stress and inflammation, as CBD normalizes the release of glutamate and cytokines as well as the induction of iNOS and COX-2 [20]. Surprisingly, we found that co-incubation of CBD with the CB2 receptor antagonist AM-630 abolished all these protective effects, suggesting that CB2 receptors are somehow involved in neuroprotective effects of CBD in immature brain [20]. In addition, adenosine receptors, in particular A2A receptors, seem to be also involved in these neuroprotective effects of CBD in the immature brain as revealed by the fact that the effect of CBD in this model was abolished by co-incubation with the A2A receptor antagonist SCH58261 [20]. CBD has been tested further in an in vivo model of NHIBD in newborn pigs, which closely resembles the actual human condition. In this model, the administration of CBD after the HI insult also reduces immediate brain damage by modulating cerebral haemodynamic impairment and brain metabolic derangement, and preventing the appearance of brain oedema and seizures. These neuroprotective effects are not only free from side effects but also associated with some beneficial cardiac, haemodynamic and ventilatory effects [84]. These protective effects restore neurobehavioural performance in the following 72 h post HI [85].
CBD and Huntington’s Disease
HD is an inherited neurodegenerative disorder caused by a mutation in the gene encoding the protein huntingtin. The mutation consists of a CAG triplet repeat expansion translated into an abnormal polyglutamine tract in the amino-terminal portion of huntingtin, which due to a gain of function becomes toxic for specific striatal and cortical neuronal subpopulations, although a loss of function in mutant huntingtin has been also related to HD pathogenesis (see [86] for review). Major symptoms include hyperkinesia (chorea) and cognitive deficits (see [87] for review). At present, there is no specific pharmacotherapy to alleviate motor and cognitive symptoms and/or to arrest/delay disease progression in HD. Thus, even though a few compounds have produced encouraging effects in preclinical studies (i.e. minocycline, coenzyme Q10, unsaturated fatty acids, inhibitors of histone deacetylases) none of the findings obtained in these studies have yet led on to the development of an effective medicine [88]. Importantly, therefore, following on from an extensive preclinical evaluation using different experimental models of HD, clinical tests are now being performed with cannabinoids, and this includes the use of CBD combined with Δ9-THC [26]. To get here, CBD was first studied in rats lesioned with 3-nitropropionic acid, a mitochondrial toxin that replicates the complex II deficiency characteristic of HD patients and that provokes striatal injury by mechanisms that mainly involve the Ca++-regulated protein calpain and generation of ROS. Neuroprotective effects in this experimental model were found with CBD alone [21] or combined with Δ9-THC as in Sativex®[22], and in both cases, these effects were not blocked by selective antagonists of either CB1 or CB2 receptors, thus supporting the idea that these effects are caused by the anti-oxidant and cannabinoid receptor-independent properties of these phytocannabinoids. It is possible, however, that this anti-oxidant/neuroprotective effect of phytocannabinoids involves the activation of signalling pathways implicated in the control of redox balance (i.e. nrf-2/ARE), as mentioned before. CBD has also been studied in rats lesioned with malonate, a model of striatal atrophy that involves mainly glial activation, inflammatory events and activation of apoptotic machinery. CBD alone did not provide protection in this model as only CB2 receptor agonists were effective [89], but the combination of CBD with Δ9-THC used in Sativex® was highly effective in this model, by preserving striatal neurons, and this protective effect involved both CB1 and CB2 receptors [23]. It is interesting to note that Δ9-THC alone produced biphasic effects in this model whereas CB1 receptor blockade aggravated the striatal damage [90]. We are presently studying the efficacy of this phytocannabinoid combination in a transgenic murine model of HD, i.e. R6/2 mice, in which the activation of both CB1 and CB2 receptors has already been found to induce beneficial effects [91, 92]. This solid preclinical evidence has provided substantial support for the evaluation of Sativex®, or equivalent cannabinoid-based medicines, as a new disease-modifying therapy in HD patients. Previous clinical studies had already used CBD, but they concentrated on symptom relief (i.e. chorea) rather than on disease progression and they did not show any significant improvement [93, 94]. We are presently engaged in a novel phase II-clinical trial with Sativex® as a disease-modifying agent in presymptomatic and early symptomatic patients [26], the outcome of which will be known soon.
CBD and Parkinson’s Disease
PD is also a progressive neurodegenerative disorder whose aetiology has been, however, associated with environmental insults, genetic susceptibility or interactions between both causes [95]. The major clinical symptoms in PD are tremor, bradykinesia, postural instability and rigidity, symptoms that result from the severe dopaminergic denervation of the striatum caused by the progressive death of dopaminergic neurons of the substantia nigra pars compacta[96]. CBD has also been found to be highly effective as a neuroprotective compound in experimental models of parkinsonism, i.e. 6-hydroxydopamine-lesioned rats, by acting through anti-oxidant mechanisms that seem to be independent of CB1 or CB2 receptors [24, 25, 97]. This observation is particularly important in the case of PD due to the relevance of oxidative injury to this disease, and because the hypokinetic profile of cannabinoids that activate CB1 receptors represents a disadvantage for this disease because such compounds can acutely enhance rather than reduce motor disability, as a few clinical data have already revealed (reviewed in [98]). Therefore, major efforts are being directed at finding cannabinoid molecules that may provide neuroprotection through their anti-oxidant properties and that may also activate CB2 receptors, but not CB1 receptors, or that may even block CB1 receptors, actions which may provide additional benefits, for example by relieving symptoms such as bradykinesia. One interesting example of a compound with this profile is the phytocannabinoid Δ9-THCV, which is presently under investigation in preclinical models of PD [25]. Thus, there could well be clinical advantages to administering Δ9-THCV together with CBD as this might induce symptomatic relief (due to the blockade of CB1 by Δ9-THCV) and neuroprotection (due to the anti-oxidant and anti-inflammatory properties of both CBD and Δ9-THCV). The combination of CBD with Δ9-THCV (rather than with Δ9-THC) would merit investigation in parkinsonian patients (reviewed in [9, 99]), as previous data obtained in clinical studies have indicated that CBD was effective in the relief of some PD-related symptoms such as dystonia, although not in others like tremor [100], but its combination with Δ9-THC, which can activate CB1 receptors, failed to improve parkinsoniam symptoms or to attenuate levodopa-induced dyskinesias [101].

Dr. Alex Jimenez’s Insight
Because the number of neurodegenerative diseases are likely to continue to grow as time passes, the race is on to discover effective treatment options for these debilitating conditions. The choices available today are restricted in scope, and therefore are typically costly. They also have side effects which should be carefully considered. Many of the most common drugs and/or medications used for Parkinson’s disease and Alzheimer’s disease cause nausea, vomiting, digestive issues, and decreased appetite, just to mention a couple. However, the use of cannabidiol, or CBD, is demonstrated to provide many health benefits without the harmful side-effects of many of these drugs and/or medications. It’s essential for healthcare professionals and researchers to continue in the search for evidence regarding the use of CBD for neurodegenerative diseases.
Concluding Remarks and Futures Perspectives
The experimental evidence presented in this review supports the idea that, from a pharmaceutical point of view, CBD is an unusually interesting molecule. As presented above, its actions are channeled through several biochemical mechanisms and yet it causes essentially no undesirable side effects and its toxicity is negligible [2]. It has shown valuable activities in numerous pharmaceutically important areas: (i) it is a potent anti-oxidant [73], which may partly explain its neuroprotective effects in PD [24, 25], and possibly in cerebral ischaemia-reperfusion (reviewed in [83]), (ii) it has been evaluated in human epileptic patients with very positive results [7–9], (iii) it has shown activity in mice with several autoimmune diseases, i.e. type-1 diabetes [102] and rheumatoid arthritis [103], (iv) it lowers the effects of myocardial ischaemic-reperfusion injury in mice [104], (v) it reduces microglial activation in mice and hence may slow the progression of Alzheimer’s disease [78], (vi) it protects against hepatic ischaemia/reperfusion injury in animals [105] and has shown considerable activity in an animal model of hepatic encephalopathy [106], (vii) it even lowers anxiety (in humans) [107] and (viii) it is already in use, together with Δ9-THC, in a buccal spray (Sativex®) to lower symptoms of multiple sclerosis [6]. The presence of CBD in Sativex® enhances the positive effects of Δ9-THC whilst reducing its adverse effects, in concordance with previous data that indicated that CBD alters some of the effects of Δ9-THC, i.e. it lowers the acute memory-impairing effects and anxiety produced by Δ9-THC [108]. In addition, cannabis with high CBD content presumably leads to fewer psychotic experiences than cannabis with a highest proportion of Δ9-THC [17].
It is possible that CBD has not become a licensed medicine (except in Sativex®) because of patenting problems. However, commercial issues apart, CBD has tremendous potential as a new medicine. Thus, because the mechanisms that underlie its anti-inflammatory effects are different from those of prescribed drugs, it could well prove to be of considerable benefit to a large number of patients, who for various reasons are not sufficiently helped by existing drugs. In type 1-diabetes, we have shown that in mice CBD very significantly lowers the number of insulin-producing cells that are affected even after the disease has advanced [102]. Its neuroprotective effects are extremely valuable as no drugs exist that have similar properties. Surprisingly very few CBD derivatives have been evaluated and compared with CBD. At least one of them, CBD-dimethylheptyl-7-oic acid, is more potent than CBD as an anti-inflammatory agent [109]. Aren’t we missing a valuable new pathway to a family of very promising new therapeutic agents?
Acknowledgments
The experimental work carried out by our group and that has been mentioned in this review article, has been supported during the last years by grants from CIBERNED (CB06/05/0089), MICINN (SAF2009-11847), CAM (S2011/BMD-2308) and GW Pharmaceuticals Ltd. The authors are indebted to all colleagues who contributed in this experimental work and to Yolanda García-Movellán for administrative support.
Competing Interests
JFR, OS and CG are supported by GW Pharma for research on phytocannabinoids and motor disorders. JMO and MRP have received funds for research from GW Pharma, Ltd. RP’s research is supported in part by funding from GW Pharmaceuticals. RM is a consultant of GW Pharma.
Cannabis, the Endocannabinoid System and Good Health
As healthcare professionals continue to sort through the emerging research studies of cannabis and cannabinoids, one thing remains clear: a more functional endocannabinoid system is fundamental for overall health and wellness. From embryonic implantation on the walls of our mother’s uterus, to nursing and growth, to reacting to injuries, endocannabinoids help us survive in a quickly changing and increasingly hostile atmosphere. As a result, many researchers began to wonder, can an individual enrich their endocannabinoid system by taking supplemental cannabis? Beyond treating symptoms, beyond even curing disease, can cannabis help us prevent disease and promote health by sparking a system that is hard-wired into most people?
Research studies have demonstrated that small doses of cannabinoids from cannabis can indicate the body to create more endocannabinoids and construct more cannabinoid receptors. That is why many first-time cannabis users do not feel a consequence, but by their second or third time working with the herb they have assembled more cannabinoid receptors and are ready to respond. More receptors raise a person’s sensitivity to cannabinoids; smaller doses have bigger impacts, and the patient has an enhanced baseline of endocannabinoid activity. Healthcare professionals believe that small, regular doses of cannabis may function as a tonic to our most central physiologic therapeutic system.
Unlike artificial derivatives, herbal cannabis may contain over one hundred distinct cannabinoids, including THC, which all work synergistically to produce better medical effects and less side effects than THC alone. While cannabis is safe and works well when smoked, most patients prefer to avoid respiratory irritation and instead use a vaporizer, cannabis tincture, or topical salve. Scientific inquiry and patient testimonials indicate that herbal cannabis has superior medical qualities to synthetic cannabinoids. Of course, we want more human-based research analyzing the effectiveness of cannabis, but the evidence base is currently large and growing continuously, despite the DEA’s best efforts to dissuade cannabis-related research.
People today need safe, natural and inexpensive remedies that stimulate our bodies’ ability to self-heal and assist our population to enhance the quality of life. Medical cannabis is just one such option. The purpose of this article has been to spread the knowledge and assist to educate patients and healthcare professionals around the evidence behind the medical use of cannabis and cannabinoids and its health benefits, including its effects on neurodegenerative disorders. Information referenced from the National Center for Biotechnology Information (NCBI). The scope of our information is limited to chiropractic as well as to spinal injuries and conditions. To discuss the subject matter, please feel free to ask Dr. Jimenez or contact us at 915-850-0900 .
Curated by Dr. Alex Jimenez
Additional Topics: Back Pain
Back pain is one of the most prevalent causes for disability and missed days at work worldwide. As a matter of fact, back pain has been attributed as the second most common reason for doctor office visits, outnumbered only by upper-respiratory infections. Approximately 80 percent of the population will experience some type of back pain at least once throughout their life. The spine is a complex structure made up of bones, joints, ligaments and muscles, among other soft tissues. Because of this, injuries and/or aggravated conditions, such as herniated discs, can eventually lead to symptoms of back pain. Sports injuries or automobile accident injuries are often the most frequent cause of back pain, however, sometimes the simplest of movements can have painful results. Fortunately, alternative treatment options, such as chiropractic care, can help ease back pain through the use of spinal adjustments and manual manipulations, ultimately improving pain relief.

EXTRA IMPORTANT TOPIC: Lower Back Pain Management
MORE TOPICS: EXTRA EXTRA: Chronic Pain Care Center
[/et_pb_text][et_pb_accordion _builder_version=”3.10″][et_pb_accordion_item _builder_version=”3.10″ title=”Blank” use_background_color_gradient=”off” background_color_gradient_start=”#2b87da” background_color_gradient_end=”#29c4a9″ background_color_gradient_type=”linear” background_color_gradient_direction=”180deg” background_color_gradient_direction_radial=”center” background_color_gradient_start_position=”0%” background_color_gradient_end_position=”100%” background_color_gradient_overlays_image=”off” parallax=”off” parallax_method=”on” background_size=”cover” background_position=”center” background_repeat=”no-repeat” background_blend=”normal” allow_player_pause=”off” background_video_pause_outside_viewport=”on” text_shadow_style=”none” box_shadow_style=”none” custom_css_main_element=”display:none;” /][et_pb_accordion_item _builder_version=”3.10″ title=”References” use_background_color_gradient=”off” background_color_gradient_start=”#2b87da” background_color_gradient_end=”#29c4a9″ background_color_gradient_type=”linear” background_color_gradient_direction=”180deg” background_color_gradient_direction_radial=”center” background_color_gradient_start_position=”0%” background_color_gradient_end_position=”100%” background_color_gradient_overlays_image=”off” parallax=”off” parallax_method=”on” background_size=”cover” background_position=”center” background_repeat=”no-repeat” background_blend=”normal” allow_player_pause=”off” background_video_pause_outside_viewport=”on” text_shadow_style=”none” box_shadow_style=”none”]
[/et_pb_accordion_item][et_pb_accordion_item _builder_version=”3.10″ title=”Close Accordion” use_background_color_gradient=”off” background_color_gradient_start=”#2b87da” background_color_gradient_end=”#29c4a9″ background_color_gradient_type=”linear” background_color_gradient_direction=”180deg” background_color_gradient_direction_radial=”center” background_color_gradient_start_position=”0%” background_color_gradient_end_position=”100%” background_color_gradient_overlays_image=”off” parallax=”off” parallax_method=”on” background_size=”cover” background_position=”center” background_repeat=”no-repeat” background_blend=”normal” allow_player_pause=”off” background_video_pause_outside_viewport=”on” open_toggle_background_color=”#ffffff” closed_toggle_background_color=”#ffffff” text_shadow_style=”none” custom_padding=”0px|||” custom_padding_tablet=”0px|||” custom_padding_phone=”0px|||” box_shadow_style=”none” custom_css_main_element=”border:none;” custom_css_toggle_title=”font-size:0.8em;” custom_css_toggle_icon=”display:none;” /][/et_pb_accordion][/et_pb_column][/et_pb_row][/et_pb_section]
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card




Comments are closed.