Can physical therapies help treat a high steppage gait from injury or medical conditions and restore normal gait patterns for individuals who have or are developing one?

Table of Contents
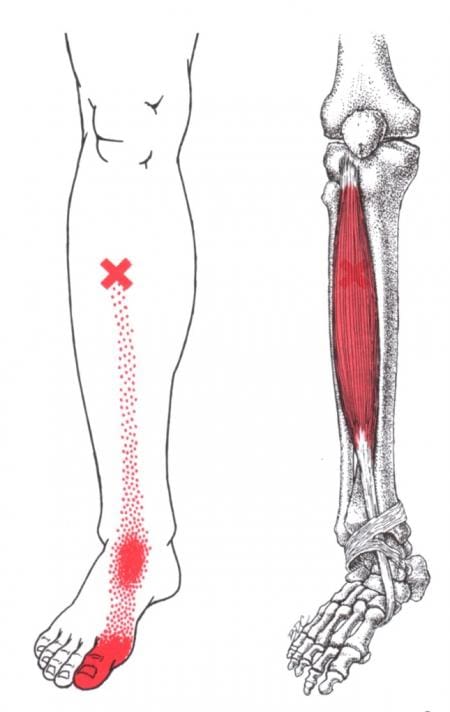
Neuropathic Gait
Neuropathic gait, aka equine or high steppage gait, is a type of walking abnormality that causes individuals to raise their hips to lift their legs higher than normal. It occurs when individuals have a foot drop or ankle equinus due to loss of dorsiflexion. As a result, the foot hangs with the toes pointing down, causing the toes to drag while walking. The foot may appear floppy when it drops. Foot drop is caused by weakness or paralysis of the anterior tibialis muscle in front of the shin bone. The anterior tibialis muscle contracts to help flex the foot and ankle while walking, ensuring the foot clears the floor and doesn’t drag. Individuals with anterior tibialis weakness or paralysis may have a neuropathic gait and excessively bend the hip and knee while stepping forward, lifting their leg high off the floor to clear the foot to avoid tripping. A physical therapy team can help with a high steppage gait pattern after illness or injury.
 Causes
Causes
Conditions that can cause anterior tibialis weakness or paralysis and a high steppage gait pattern include:
Sciatica
- Pain caused by compression or irritation of the sciatic nerve starts in the lower back and travels down the back of the leg. (McCabe, F. J., McCabe, J. P. 2016)
Peroneal Nerve Injury
- Damage to the peroneal nerve branches from the sciatic nerve that help move the lower leg and foot. (Johns Hopkins Medicine. 2024)
Multiple Sclerosis
- An autoimmune disease that damages nerve cells in the brain and spinal cord. (Taylor, P. N. et al., 2016)
Stroke
- Interruption of blood circulation to part of the brain can cause disability. (Kaykisiz, E. K., Unluer, E. E. 2017)
A primary healthcare provider may refer a physical therapy team to help correct the neuropathic gait pattern.
Treatment
Treatment can involve various therapies that focus on the anterior tibialis muscle.
- Targeted ankle exercises can help strengthen the muscle.
- Calf stretches can help maintain the ankle’s range of motion.
- Gait training exercises.
- Balance exercises will help improve overall proprioception, or the sense of the body’s position and movement.
- Neuromuscular electrical stimulation, or NMES, can help improve the function of the muscle. (Hollis, S., McClure, P. 2017)
- The electrical stimulation artificially contracts the muscle to restore proper function.
- For anterior tibialis weakness caused by sciatica, back decompression exercises may be prescribed to relieve pressure off the sciatic nerve.
- The exercises release the nerve to restore normal signal transmission up and down the nerve in the lower back.
- Neuromuscular electrical stimulation may also be used to help improve muscle function.
Assistive Walking Devices
A therapist may suggest using an assistive device to help the patient walk properly. This could include a wheeled walker or a quad cane. A temporary solution to anterior tibialis weakness is to elevate the foot while walking with an elastic band. Tie a band around the leg below the knee and secure it around the ball of the foot. When swinging the leg forward, the band pulls the foot up. Using it as a temporary solution may help maintain safe mobility. Sometimes, paralysis of the anterior tibialis muscle can become permanent. In this case, individuals may benefit from a special brace called an ankle-foot orthosis. The brace helps to lift the foot and toes off the ground.
For individuals concerned about losing their balance and falling, there are ways to improve walking patterns to stay safe. A healthcare provider may recommend physical therapy to correct gait, strengthen the anterior tibialis muscle, improve balance, and educate on injury prevention. Individuals should discuss symptoms and conditions with a primary physician, healthcare provider, or specialist to guide them in the right direction and determine the best treatment.
Injury Medical Chiropractic and Functional Medicine Clinic uses an integrated approach personalized to the individual that focuses on what works for them and treats injuries and chronic pain syndromes through personalized care plans that improve ability through flexibility, mobility, and agility programs to relieve pain. If other treatment is needed, Dr. Jimenez has teamed up with top surgeons, clinical specialists, medical researchers, and rehabilitation providers to provide the most effective treatments.
Control Foot Motion and Posture
References
McCabe, F. J., & McCabe, J. P. (2016). An Unusual Presentation of Right-Sided Sciatica with Foot Drop. Case reports in orthopedics, 2016, 9024368. doi.org/10.1155/2016/9024368
Johns Hopkins Medicine. (2024). Peroneal nerve injury. www.hopkinsmedicine.org/health/conditions-and-diseases/peroneal-nerve-injury
Kaykisiz, E. K., & Unluer, E. E. (2017). An Unexpected Reason for Isolated Foot Drop: Acute Stroke. Pakistan journal of medical sciences, 33(5), 1288–1290. doi.org/10.12669/pjms.335.13593
Taylor, P. N., Wilkinson Hart, I. A., Khan, M. S., & Slade-Sharman, D. E. (2016). Correction of Footdrop Due to Multiple Sclerosis Using the STIMuSTEP Implanted Dropped Foot Stimulator. International journal of MS care, 18(5), 239–247. doi.org/10.7224/1537-2073.2015-038
Hollis, S., & McClure, P. (2017). Intramuscular Electrical Stimulation for Muscle Activation of the Tibialis Anterior After Surgical Repair: A Case Report. The Journal of orthopaedic and sports physical therapy, 47(12), 965–969. doi.org/10.2519/jospt.2017.7368
Post Disclaimer
Professional Scope of Practice *
The information herein on "Preventing and Treating Neuropathic Gait: A Comprehensive Guide" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Wellness blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-C) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on dralexjimenez.com, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.*
Our office has reasonably attempted to provide supportive citations and has identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card



 Causes
Causes