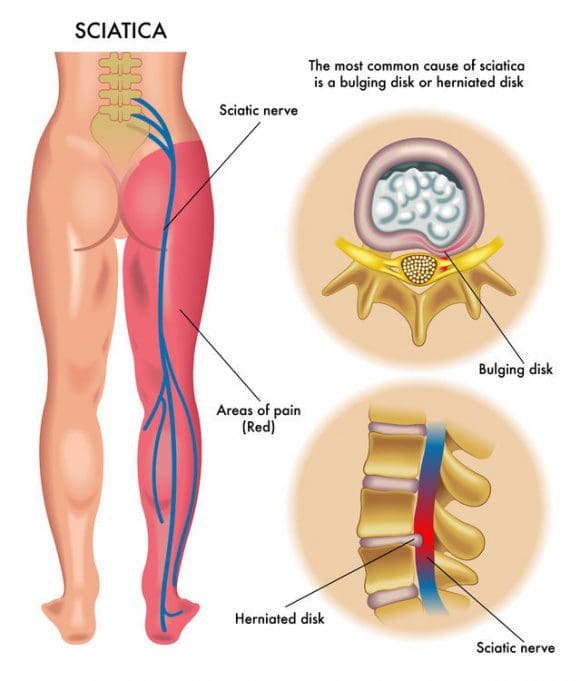
Cause Of Sciatica: Several lumbar spine (lower back) disorders can cause sciatica. Sciatica is often described as mild to intense pain in the left or right leg. Sciatica is caused by compression of one or more of the 5 sets of nerve roots in the lower back. Sometimes doctors call sciatica a radiculopathy. Radiculopathy is a medical term used to describe pain, numbness, tingling, and weakness in the arms or legs caused by a nerve root problem. If the nerve problem is in the neck, it is called a cervical radiculopathy. However, since sciatica affects the low back, it is called a lumbar radiculopathy.
Table of Contents
Pathways To Sciatic Nerve Pain
Five sets of paired nerve roots in the lumbar spine combine to create the sciatic nerve. Starting at the back of the pelvis (sacrum), the sciatic nerve runs from the back, under the buttock, and downward through the hip area into each leg. Nerve roots are not “solitary” structures but are part of the body’s entire nervous system capable of transmitting pain and sensation to other parts of the body. Radiculopathy occurs when compression of a nerve root from a disc rupture (herniated disc) or bone spur (osteophyte) occurs in the lumbar spine prior to it joining the sciatic nerve.
 What Causes Sciatic Nerve Compression?
What Causes Sciatic Nerve Compression?
Several spinal disorders can cause spinal nerve compression and sciatica or lumbar radiculopathy. The 6 most common are:
- a bulging or herniated disc
- lumbar spinal stenosis
- spondylolisthesis
- trauma
- piriformis syndrome
- spinal tumors
Sciatica Cause: 6 Leading Sources
Several lumbar spine (lower back) disorders can cause sciatica. Sciatica is often described as mild to intense pain in the left or right leg. Sciatica is caused by compression of one or more of the 5 sets of nerve roots in the lower back. Sometimes doctors call sciatica a radiculopathy. Radiculopathy is a medical term used to describe pain, numbness, tingling, and weakness in the arms or legs caused by a nerve root problem. If the nerve problem is in the neck, it is called a cervical radiculopathy. However, since sciatica affects the low back, it is called a lumbar radiculopathy.
Sciatica Cause #1: Lumbar Bulging Disc Or Herniated Disc
A bulging disc is also known as a contained disc disorder. This means the gel-like center (nucleus pulposus) remains “contained” within the tire-like outer wall (annulus fibrosus) of the disc.
A herniated disc occurs when the nucleus breaks through the annulus fibrosus. It is called a “non-contained” disc disorder. Whether a disc bulges or herniates, disc material can press against an adjacent nerve root and compress delicate nerve tissue and cause sciatica.
The consequences of a herniated disc are worse. Not only does the herniated disc cause direct compression of the nerve root against the interior of the bony spinal canal, but the disc material itself also contains an acidic, chemical irritant (hyaluronic acid) that causes nerve inflammation. In both cases, nerve compression and irritation cause inflammation and pain, often leading to extremity numbness, tingling, and muscle weakness.
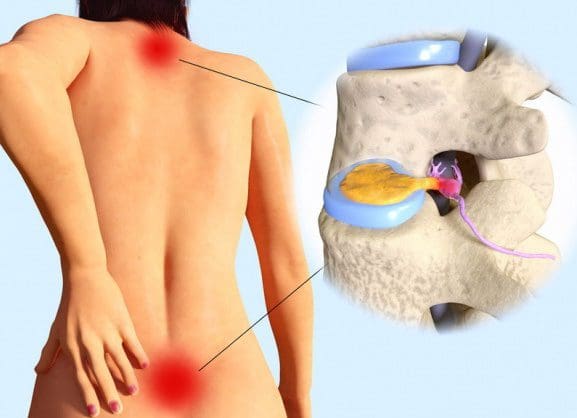
Herniated disc is a relatively common condition that can occur anywhere along the spine, but most often affects the lower back or neck region. Also known as a slipped disc or ruptured disc, a herniated disc develops when one of the cushion-like pads between the vertebrae moves out of position and presses on adjacent nerves.
Herniated discs are typically caused by overuse injuries or trauma to the spine; however, disc conditions can also develop as a result of the normal aging process. It is also known that there is a genetic factor that contributes to the development of disc degeneration and herniated disc. In most cases, a herniated disc in the lower back will heal within six months, as the size of herniation shrinks with time via resorption. Surgery may be needed if medication, physical therapy and other treatments fail.
What Is A Disc?
Spinal discs are cushion-like pads located between the vertebrae. Without these “shock absorbers,” the bones in the spine would grind against one another. In addition to giving the spine flexibility and making movements such as twisting and bending possible, discs protect the spine by absorbing the impact of trauma and body weight. Each disc has a strong outer layer called annulus fibrosus and a soft, gel-like center, called nucleus pulposus. There are fibers on the outside of each disc that attach to adjacent vertebrae and hold the disc in place. A herniated disc occurs when the outer layer tears or ruptures and the gel-like center leaks into the spinal canal.
The spinal canal has just enough space to house the spinal cord and spinal fluid. When a disc herniates and spills into the spinal canal, it can cause compression of the nerves or spinal cord. Intense, debilitating pain and alterations in sensation often occur. In addition, the gel-like substance inside the disc releases chemical irritants that contribute to nerve inflammation and pain.
What Causes A Herniated Disc?
As we age, the spinal discs gradually lose fluid volume. This process starts at about age 30 and progresses slowly, over time. As the discs dry out, microscopic cracks or tears can form on the outer surface, causing it to become brittle, weak and more susceptible to injury. The most common causes of herniated disc are:
- Wear and tear: Discs dry out and aren’t as flexible as they once were.
- Repetitive movements: Work, lifestyle, and certain sports activities that put stress on the spine, especially the lower back, further weaken an already vulnerable area.
- Lifting the wrong way: Never lift while bent at the waist. Proper lifting entails lifting with your legs and a straight back.
- Injury: High-impact trauma can cause the disc to bulge, tear or rupture.
- Obesity: Carrying excess weight puts an undue amount of strain on the spine.
- Genetics: There are some genes that are more commonly present in individuals with disc degeneration. More research is needed to investigate the role of these genes—they could be targets of biological treatment in the future.
What Are The Symptoms Of A Herniated Disc?
Pain from a herniated disc can vary, depending on the location and severity of the injury. It is typically felt on one side of the body.
If the injury is minimal, little or no pain may be felt. If the disc ruptures, pain can be severe and unrelenting. Pain may radiate to an extremity in a specific nerve root distribution if significant nerve impingement has occurred. For example, sciatica is frequently caused by a herniated disc in the lower back. Herniated disc can manifest itself with a range of symptoms, including:
- Dull ache to severe pain
- Numbness, tingling, burning
- Muscle weakness; spasm; altered reflexes
- Loss of bowel or bladder control (Note: These symptoms constitute a medical emergency. If they occur, seek medical attention immediately).
How Is A Herniated Disc Diagnosed?
History and physical examination point to a diagnosis of herniated disc. A herniated disc is likely if low back pain is accompanied by radiating leg pain in a nerve root distribution with positive straight leg raising test (ie, elevating the leg while lying down causes radiating pain down the leg), and other neurologic deficits such as numbness, weakness, and altered reflexes.
Imaging studies are usually ordered to confirm a diagnosis of herniated disc. X-rays are not the imaging medium of choice because soft tissues (eg, discs, nerves) are hard to capture with this technology. However, they may be used as an initial tool to rule out other disorders such as a growth or fracture. Confirmation of the suspicion of herniated disc is generally accomplished with:
- Magnetic Resonance Imaging (MRI): This technology reveals the spinal cord, surrounding soft tissue and nerves. It is the best imaging study to support the diagnosis of a herniated disc.
- Nerve Conduction Studies (NCS) and Electromyogram (EMG): These studies use electrical impulses to measure the degree of damage to the nerve/s caused by compression from a herniated disc and other conditions that cause nerve impingement can be ruled out. NCS and EMG are not routine tests to diagnose herniated disc.
Herniated discs sometimes heal on their own through a process called resorption. This means that the disc fragments are absorbed by the body. Most people suffering from herniated disc respond well to conservative treatment and do not require surgery.
Sciatica Cause #2: Lumbar Spinal Stenosis
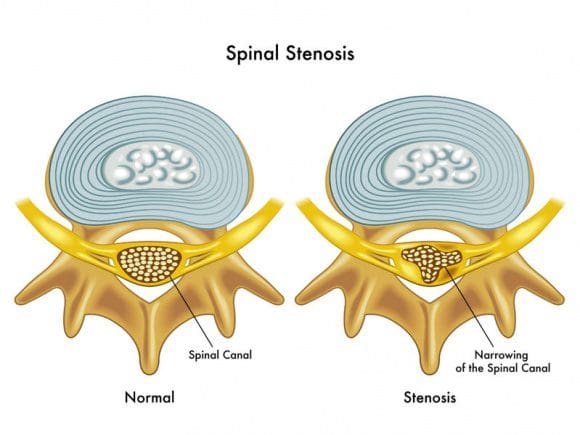 Spinal stenosis is a nerve compression disorder most often affecting older adults. Leg pain similar to sciatica may occur as a result of lumbar spinal stenosis. The pain is usually positional, often brought on by activities such as standing or walking and relieved by sitting down.
Spinal stenosis is a nerve compression disorder most often affecting older adults. Leg pain similar to sciatica may occur as a result of lumbar spinal stenosis. The pain is usually positional, often brought on by activities such as standing or walking and relieved by sitting down.
Spinal nerve roots branch outward from the spinal cord through passageways called neural foramina comprised of bone and ligaments. Between each set of vertebral bodies, located on the left and right sides, is a foramen. Nerve roots pass through these openings and extend outward beyond the spinal column to innervate other parts of the body. When these passageways become narrow or clogged causing nerve compression, the term foraminal stenosis is used.
What Is Spinal Stenosis?
A clue to answering this question is found in the meaning of each word. Spinal refers to the spine. Stenosis is a medical term used to describe a condition where a normal-size opening has become narrow. Spinal stenosis may affect the cervical (neck), thoracic (chest), or lumbar (lower back) spines.
The most commonly area affected is the lumbar spine followed by the cervical spine.
Visualize Spinal Stenosis?
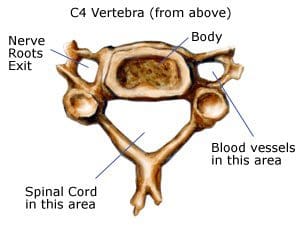
Consider a water pipe. Over time, rust and debris builds up on the walls of the pipe, thereby narrowing the passageway that normally allows water to freely flow. In the spine, the passageways are the spinal canal and the neuroforamen. The spinal canal is a hollow vertical hole that contains the spinal cord. The neuroforamen are the passageways that are naturally created between the vertebrae through which spinal nerve roots exit the spinal canal.
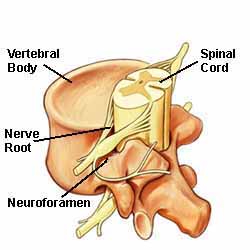 The neuroforamen are the passageways that are naturally created between the vertebrae through which spinal nerve roots exit the spinal canal.
The neuroforamen are the passageways that are naturally created between the vertebrae through which spinal nerve roots exit the spinal canal.
Illustration above: The spine’s bony structures encase and protect the spinal cord. Small nerve roots shoot off from the spinal cord and exit the spinal canal through passageways called neuroforamen.
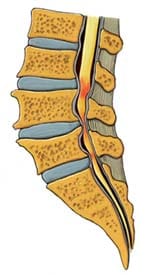
Lumbar (low back) spinal stenosis is illustrated below. Notice the narrowed areas in the spinal canal (reddish-colored areas). As the canal space narrows, the spinal cord and nearby nerve roots are squeezed causing different types of symptoms. The medical term is nerve compression.
 Anatomy Overview Can Help You Understand Spinal Stenosis
Anatomy Overview Can Help You Understand Spinal Stenosis
The spine is a column of connected bones called vertebrae. There are 24 vertebrae in the spine, plus the sacrum and tailbone (coccyx). Most adults have 7 vertebrae in the neck (the cervical vertebrae), 12 from the shoulders to the waist (the thoracic vertebrae), and 5 in the lower back (the lumbar vertebrae). The sacrum is made up of 5 vertebrae between the hipbones that are fused into one bone. The coccyx is made up of small fused bones at the tail end of the spine.
Lamina and Spinous Processes: At the back (posterior) of each vertebra, you have the lamina, a bony plate that protects your spinal canal and spinal cord. Your vertebrae also have several bony tabs that are called spinous processes; those processes are attachment points for muscles and ligaments.
Ligaments, Especially the Ligamentum Flavum: Vertebrae are connected by ligaments, which keep the vertebrae in their proper place. The ligamentum flavum is a particularly important ligament. Not only does it help stabilize your spine, it also protects your spinal cord and nerve roots. Plus, the ligamentum flavum is the strongest ligament in your spine.
The ligamentum flavum is a dynamic structure, which means that it adapts its shape as you move your body. When you’re sitting down and leaning forward, the ligamentum flavum is stretched out; that gives your spinal canal more room for the spinal nerves. When you stand up and lean back, though, the ligamentum flavum becomes shorter and thicker; that means there’s less room for the spinal nerves. (This dynamic capability helps explain why people with spinal stenosis find that sitting down feels better than standing or walking.)
Discs: In between each vertebra are tough fibrous shock-absorbing pads called the intervertebral discs. Each disc is made up of a tire-like outer band (annulus fibrosus) and a gel-like inner substance (nucleus pulposus).
Spinal Nerves and the Spinal Cord: Nerves are also an important part of your spinal anatomy—after all, they’re what sends messages from your brain to the rest of your body. The spinal cord, the thick bundle of nerves that extends downward from the brain, passes through a ring in each vertebra. Those rings line up into a channel called the spinal canal.
Between each vertebra, two nerves branch out of the spinal cord (one to the right and one to the left). Those nerves exit the spine through openings called the foramen and travel to all parts of your body.
 Normally, the spinal channel is wide enough for the spinal cord, and the foramen are wide enough for the nerve roots. But either or both can become narrowed, and cause spinal stenosis.
Normally, the spinal channel is wide enough for the spinal cord, and the foramen are wide enough for the nerve roots. But either or both can become narrowed, and cause spinal stenosis.
Sciatica Cause #3: Spondylolisthesis
Spondylolisthesis is a disorder that most often affects the lumbar spine. It is characterized by one vertebra slipping forward over an adjacent vertebra. When a vertebra slips and is displaced, spinal nerve root compression occurs and often causes sciatic leg pain. Spondylolisthesis is categorized as developmental (found at birth, develops during childhood) or acquired from spinal degeneration, trauma or physical stress (eg, lifting weights).
Spondylolisthesis occurs when one vertebra slips forward over the vertebra below it. The term is pronounced spondy-low-lis-thesis and is derived from the Greek language: spondylo means vertebra and listhesis means to slip. There are several types or causes of spondylolisthesis; a few are listed below.
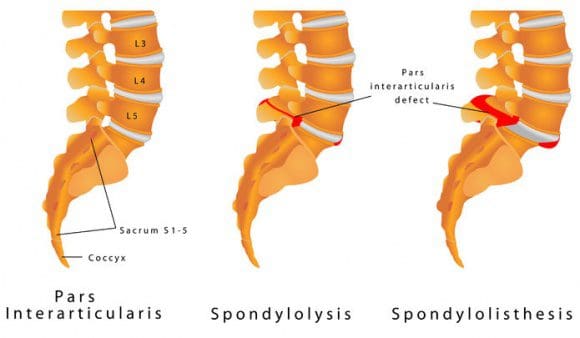
- Congenital spondylolisthesis means the disorder is present at birth.
- Isthmic spondylolisthesis occurs when a defect, such as a fracture occurs in a bony supporting vertebral structure at the back of the spine.
- Degenerative spondylolisthesis is more common and is often associated with degenerative disc disease, wherein the discs (eg, due to the effects of growing older) lose hydration and resilency.
How Spondylolisthesis May Develop
The lumbar spine is exposed to directional pressures while it carries, absorbs, and distributes most of your body’s weight at rest and during activity. In other words, while your lumbar spine is carrying and absorbing body weight, it also moves in different directions (eg, rotate, bend forward). Sometimes, this combination causes excessive stress to the vertebra and/or its supporting structures, and may lead to a vertebral body slipping forward over the vertebrae beneath.
Who May Be At Risk
If a family member (eg, mother, father) has spondylolisthesis, your risk for developing the disorder may be greater. Some activities make you more susceptible to spondylolisthesis. Gymnasts, linemen in football, and weight lifters all put significant pressure and weight on their low backs. Think about gymnasts and the positions they put their body in: They practically bend in half backwards—that’s an extreme arched back. They also twist through the air quickly when doing flips and then land, absorbing the impact through their legs and low back. Those movements put substantial stress on the spine, and spondylolisthesis can develop as a result of repeated excessive strains and stress.
X-Ray View Of Spondylolisthesis
The x-ray below shows you a good example of a lumbar spondylolisthesis. Look at the area the arrow is pointing to: You can see that the vertebra above the arrow isn’t in line with the vertebra below it. It’s slipped forward; it’s spondylolisthesis.
 Arrow Points To A Lumbar Spondylolisthesis
Arrow Points To A Lumbar Spondylolisthesis
Grading Spondylolisthesis
Doctors “grade” the severity of a spondylolisthesis using five descriptive categories. Although there are several factors your doctor considers when evaluating your spondylolisthesis, the grading scale (below) is based on the far forward a vertebral body has slid forward over the vertera beneath. Often, the doctor uses a lateral (side view) x-ray to examine and grade a spondyloisthesis. Grade I is a smaller slip than Grade IV or V.
- Grade I: Less than 25% slip
- Grade II: 25% to 49% slip.
- Grade III: 50% to 74% slip.
- Grade IV: 75% to 99% slip.
- Grade V: The vertebra that has fallen forward off the vertebra below it. This is the most severe type of spondylolisthesis and is termed spondyloptosis.
Sciatica Cause #4: Trauma
Sciatica can result from direct nerve compression caused by external forces to the lumbar or sacral spinal nerve roots. Examples include motor vehicle accidents, falling down, football and other sports. The impact may injure the nerves or, occasionally, fragments of broken bone may compress the nerves.
Sciatica Cause #5: Piriformis Syndrome
Piriformis syndrome is named for the piriformis muscle and the pain caused when the muscle irritates the sciatic nerve. The piriformis muscle is located in the lower part of the spine, connects to the thighbone, and assists in hip rotation. The sciatic nerve runs beneath the piriformis muscle. Piriformis syndrome develops when muscle spasms develop in the piriformis muscle thereby compressing the sciatic nerve. It may be difficult to diagnose and treat due to the lack of x-ray or magnetic resonance imaging (MRI) findings.
If you’ve ever felt pain in the hip, pain in the center of the butt, or pain down the back of the leg, you are likely suffering, at least partially, with piriformis syndrome. The piriformis is a muscle which runs from your sacrum (mid-line base of spine) to the outer hip bone (trochanter). This muscle truly works overtime on anyone who runs at all.
 The muscles in and around the gluteal region help with three areas
The muscles in and around the gluteal region help with three areas
- rotation of the hip and leg;
- balance while one foot is off the ground; and
- stability for the pelvic region.
Needless to say, all of these characteristics are highly needed by runners (and everyone else, when you come to think of it).
Injuries To The Piriformis
This muscle is a prime candidate for repetitive motion injury (RMI). RMI occurs when a muscle is asked to perform beyond it’s level of capability, not given enough time to recover, and asked to perform again. The typical response from a muscle in this situation is to tighten, which is a defensive response of the muscle. This tightness, however, manifests itself in several ways to a runner.
The first symptom suggesting piriformis syndrome would be pain in and around the outer hip bone. The tightness of the muscle produces increased tension between the tendon and the bone which produces either direct discomfort and pain or an increased tension in the joint producing a bursitis. Again, a bursitis is an inflammation of the fluid filled sac in a joint caused by an elevation of stress and tension within that joint.
The second symptom suggesting piriformis syndrome would be pain directly in the center of the buttocks. Although this is not as common as the other two symtpoms, this pain can be elicited with direct compression over the belly of the buttocks area. A tight muscle is a sore muscle upon compression due to a reduced blood flow to that muscle.
The third symptom suggesting piriformis syndrome would be a sciatic neuralgia, or pain from the buttocks down the back of the leg and sometimes into different portions of the lower leg. We have an article that can teach you more about how piriformis syndrome and sciatica are related.
The sciatic nerve runs right through the belly of the piriformis muscle and if the piriformis muscle contracts from being overused, the sciatic nerve now becomes strangled, producing pain, tingling and numbness.
Simple Physiology
Any muscle repetitively used needs to have an opportunity to recover. This recovery can either be on Nature’s clock, or can be facilitated and sped up with proper knowledge and treatment. Since the muscle is tightening due to overuse, continued use will only make it worse. This injured muscle needs to relax and have increased blood flow encouraged to it for more rapid healing. This tightness that exists also reduces the normal blood flow going to the muscle reducing the speed with which the muscle can recover. To encourage fresh, oxygen-rich blood to the muscle is the most powerful means of getting the muscle to begin to relax and function normally. Multiple massages per day to this area is greatly encouraged.
The next step in this “recovery” process is to use a tennis ball under the butt and hip area. While sitting down on the floor, roll away from the side of involvement and place a tennis ball just inside the outer hip bone under the butt area. As you begin to allow your weight onto the tennis ball, note areas of increased pain and soreness. Trigger points will tend to accumulate in a repetitively used muscle, and until these toxins are manually broken up and eliminated, the muscle will have an artificial ceiling with regard to flexibility potential and recovery potential. So, if it’s sore and hurts while your sitting on it, you’re doing a good job. Let the ball work under each spot for 15-20 seconds before moving it to another area. Once you’ve been on the ball for 4-5 minutes, now put the ankle of the involved leg over the knee of the non-involved leg (crossing your legs). Now place the tennis ball just inside the outer hip bone again and work the tendon of the piriformis muscle. While this pain is typically excruciating and takes some time to effectively reduce, the benefits here are huge. Be patient, be consistent and good things will happen.
Additional Treatments
Due to the fact that the sciatic neuralgia and the hip bursitis or tendonitis are both inflammatory in nature, ice, or cryotherapy, over the involved area 15-20 minutes at a time will be beneficial. This should be done multiple times per day.
Stretching of the hip muscles should not be done until the acute pain is gone. At that point in time, begin with gentle stretching, such as the cross-legged stretch while pulling up on the knee. The muscle should have increased flexibility before an active return to running.
Finally, I’m always discouraging the use of pharmaceutical anti-inflammatories. Not only do they greatly aggravate the intestines, but they also suggest an artificial wellness that can lead to bigger problems. Proteolytic enzymes, such as bromelain, are both natural and extremely beneficial with no side effects.
Conclusion: The piriformis muscle is pretty important for all of us.
Sciatica Cause #6: Spinal Tumors
Spinal tumors are abnormal growths that are either benign or cancerous (malignant). Fortunately, spinal tumors are rare. However, when a spinal tumor develops in the lumbar region, there is a risk for sciatica to develop as a result of nerve compression.
If you think you have sciatica, call your doctor or chiropractor. The first step toward relieving pain is a proper diagnosis.
Written by Jean-Jacques Abitbol, MD; Reviewed by Brian R. Subach, MD
Howard S. An, MD, Stewart G. Eidelson, MD; Reviewed by Howard S. An, MD, Jason M. Highsmith, MD
Timothy J. Maggs, D.C.; Reviewed by Edward C. Benzel, MD
Check out our sister page at SPINEUNIVERSE
Chiropractic Care Benefits Juvenile Arthritis Patients
Post Disclaimer
Professional Scope of Practice *
The information herein on "Cause Of Sciatica: Six Sources" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Wellness blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-C) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on dralexjimenez.com, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.*
Our office has reasonably attempted to provide supportive citations and has identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card



 Anatomy Overview Can Help You Understand Spinal Stenosis
Anatomy Overview Can Help You Understand Spinal Stenosis