Young athletes are not simply ‘mini adults’. With that in mind, chiropractor Dr. Alexander Jimenez brings insight to the common injuries occurring at joint surfaces in young athletes, and describes how these injuries can be prevented through appropriate management of athlete development.
When treating young athletes, it is crucial that we care for them with the specificity they deserve and not just as ‘mini adults’. The recent ‘International Olympic Committee consensus statement on youth athletic development’ challenges all sporting bodies and practitioners to embrace and implement recommended principles in order to develop healthy, capable and resilient young athletes(1).
As with adults, we should take into account the load, volume, frequency and type of sport the athlete is participating in. However, to properly guide injury prevention and management, coaching and support staff should also consider the athlete’s growth phase and stage of development.
Table of Contents
Lower Limb Injuries
Lower limb injuries account for approximately 60% of the injury burden of young athletes aged 11-18(1). Although these include traumatic injuries, up to half are as a result of overuse or ‘burnout’, with running being the leading cause of this type of injury(2).
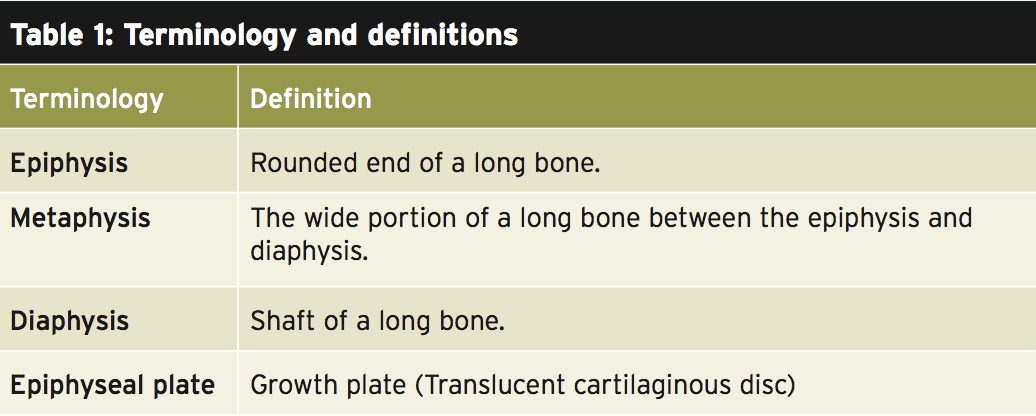
It is during pubertal growth spurts (usually occurring early – mid puberty) that the epiphyseal plate undergoes endochondral ossification, through cell proliferation to form longitudinal growth(3). When this process is completed towards the end of puberty (usually in females prior to males), final adult height is reached. (NB – see table 1 for explanation of the terminology)
 The physes in young athletes are an additional site of injury and one not seen in adults. Physes injury can occur either from a traumatic event, or commonly due to the repeated stresses of sport and overload. This most frequently occurs during pubertal growth spurts when the cells are most active and cartilage is thought to be weaker(4). The advantage of having open growth plates is they result in accelerated fracture healing and remodeling – but only if managed well.
The physes in young athletes are an additional site of injury and one not seen in adults. Physes injury can occur either from a traumatic event, or commonly due to the repeated stresses of sport and overload. This most frequently occurs during pubertal growth spurts when the cells are most active and cartilage is thought to be weaker(4). The advantage of having open growth plates is they result in accelerated fracture healing and remodeling – but only if managed well.
Growth injuries in young athletes are commonly underreported because many practitioners see them as ‘part of the course’ of growing and attempt to manage without any time loss to sport. Athletes, parents and coaches may try to conceal pain due to the risk of missing out on selections or relegation from teams.
It is important to consider this may also be the first injury a young athlete has suffered; therefore social and psychological impacts should be addressed focusing on the long-term goals of the athlete and how best to achieve this, avoiding further injury(5).
As well as an adolescent growth spurt being a risk factor for growth injuries, there is also increased risk with significant hyper and hypomobility, lack of lean tissue mass, dietary insufficiencies and vascular defects(6,7). Training variables that increase the risk include excessive repeated loading, insufficient recovery, and focus on volume and competition over skill development(8). These factors all decrease the positive adaptations that training has on the body, and leave athletes young and old at risk of injury.
Using chronological age can be a poor indicator upon which to base sport development due to the differing physical and emotional growth phases of children of the same age. For example gymnasts and dancers tend to be skeletally immature, while females generally reach maturity at an earlier age. Readiness should be the ability to match growth, motor, sensory, cognitive, social and emotional development with tasks and demands of a specific sport and the training required(2).
When diagnosing suspected epiphysis injuries, clinical examination through palpation, flexibility and resisted muscle testing (which stress the physis) should be indicators. It is important to be aware that not all epiphysis are ossified at an early stage. Therefore in areas such as ischial tuberosity, iliac crest and base of 5th metatarsal, problems are often not visible on X-ray until final growth spurts have occurred(4). Therefore, while useful in differential diagnosis, radiological investigation should not therefore be relied upon – particularly as misdiagnosis or mismanagement of epiphyseal and apophyseal injuries can lead to prolonged healing, deformity, growth changes or avulsion, leading to surgery.
Apophyseal Injury
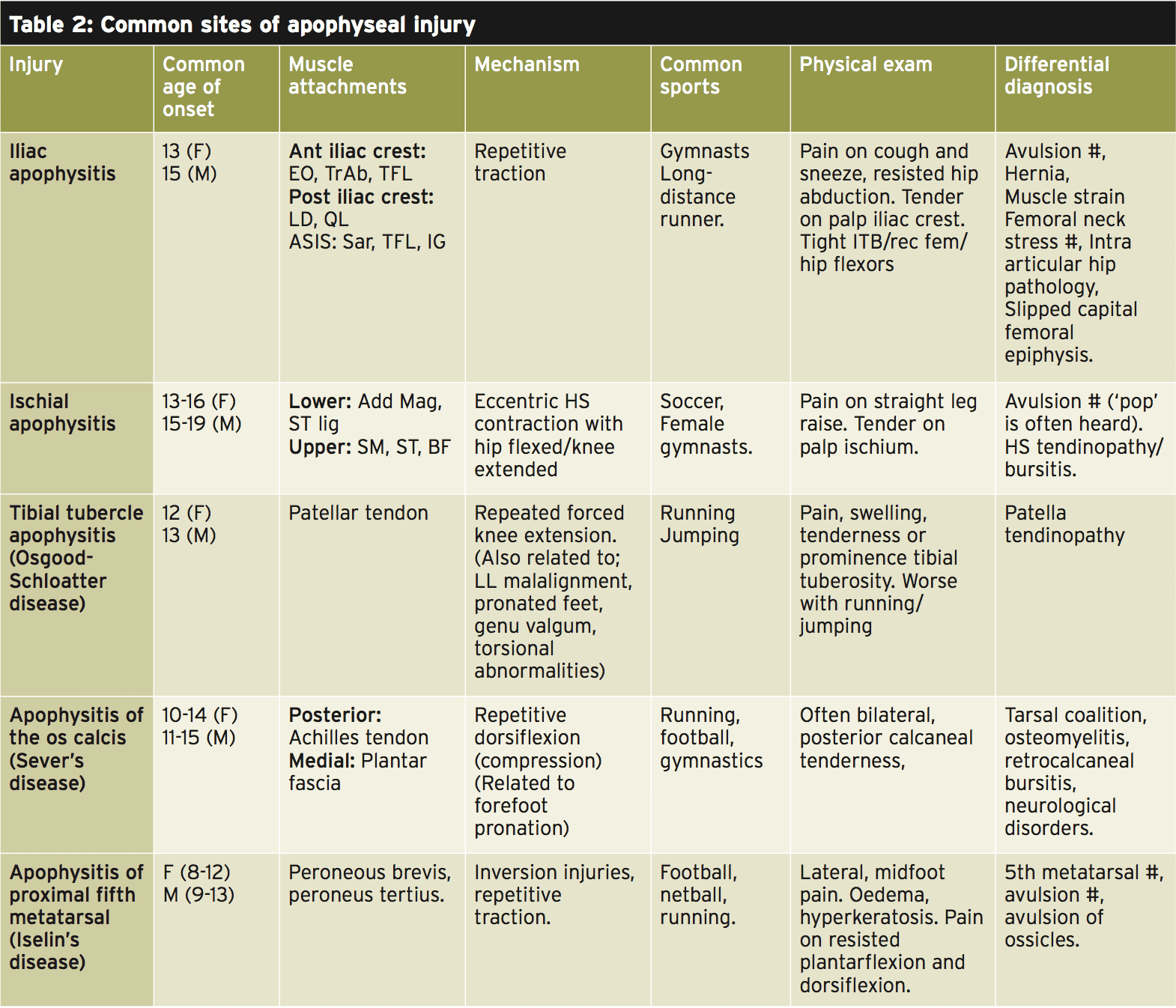
When diagnosing apophyseal injuries, knowledge of muscular attachments is paramount to early identification and differential diagnosis from commonly misdiagnosed muscle injuries. Apophyses are growth areas that have muscle attachments in close proximity. These areas do not contribute to linear growth as they are not on the joint surface, and therefore have a decreased risk of growth defects. However, they are a leading cause of injury in young athletes and account for a significant time loss to sport(7).
When apophyses are exposed to repetitive traction, they can become irritated and result in apophysitis, which if not managed, can lead to an avulsion fracture. The overload is often a response to increased training load or volume, change in sport or footwear or inadequate recovery. Table 2 (4,6,7,9) outlines the common sites where apophystitis injuries occur in developing athletes(4,6,7,9). The majority of apophyseal pain ends when the physis closes and the athlete has reached skeletal maturity(3).
Treatment for apophysitis should begin with identifying and reducing the aggravating activity/activities. Thorough education should be provided to the athlete, parent and coaches to maximize compliance in the rehabilitation process. It is important to highlight the potential secondary problems if the athlete fails to adhere to the management plan.
In all apophysitis injuries, weight bearing should be reduced, and aggravating activities initially avoided or modified until pain free. Stretching of tissues in the area should then be commenced (with the exception of athletes with Severs), followed by a strengthening program, progressing from isometric loading into bodyweight exercises, followed by graduated return to loading and specific sport training. If return to the causative repetitive action occurs too soon, the athlete is at risk of avulsion or further irritation.
In athletes with Osgood Schlatter’s disease, good adherence to physiotherapy has shown reduced enlargement of the tibial tuberosity. If there is ongoing discomfort post-epiphyseal fusion at skeletal maturity, the removal of ossicles formed during the repetitive traction can decrease discomfort. Poor management of Sever’s disease can lead to increased risk of metaphysis stress fractures – therefore adherence to 3-4 weeks of activity avoidance (or immobilisation if compliance is poor) is paramount, and linked to a quicker return to sport(4).
Orthotics, heel raises and footwear assessment are also useful adjuncts for these athletes – in conjunction with soft tissue release and strengthening. Stretching is likely to aggravate Severs pain further due to compression over the apophyseal site. Iselin’s can also lead to an increased risk of stress reaction – therefore a short period (2-4 weeks) in a short-leg boot is recommended to minimise risk of fractures of the 5th metatarsal. The progression of home exercises is similar to those given following an acute ankle sprain(6). If avulsion is suspected, athletes should undergo further investigation and consult with a surgeon for advice regarding surgical management.
Epiphyseal Injury
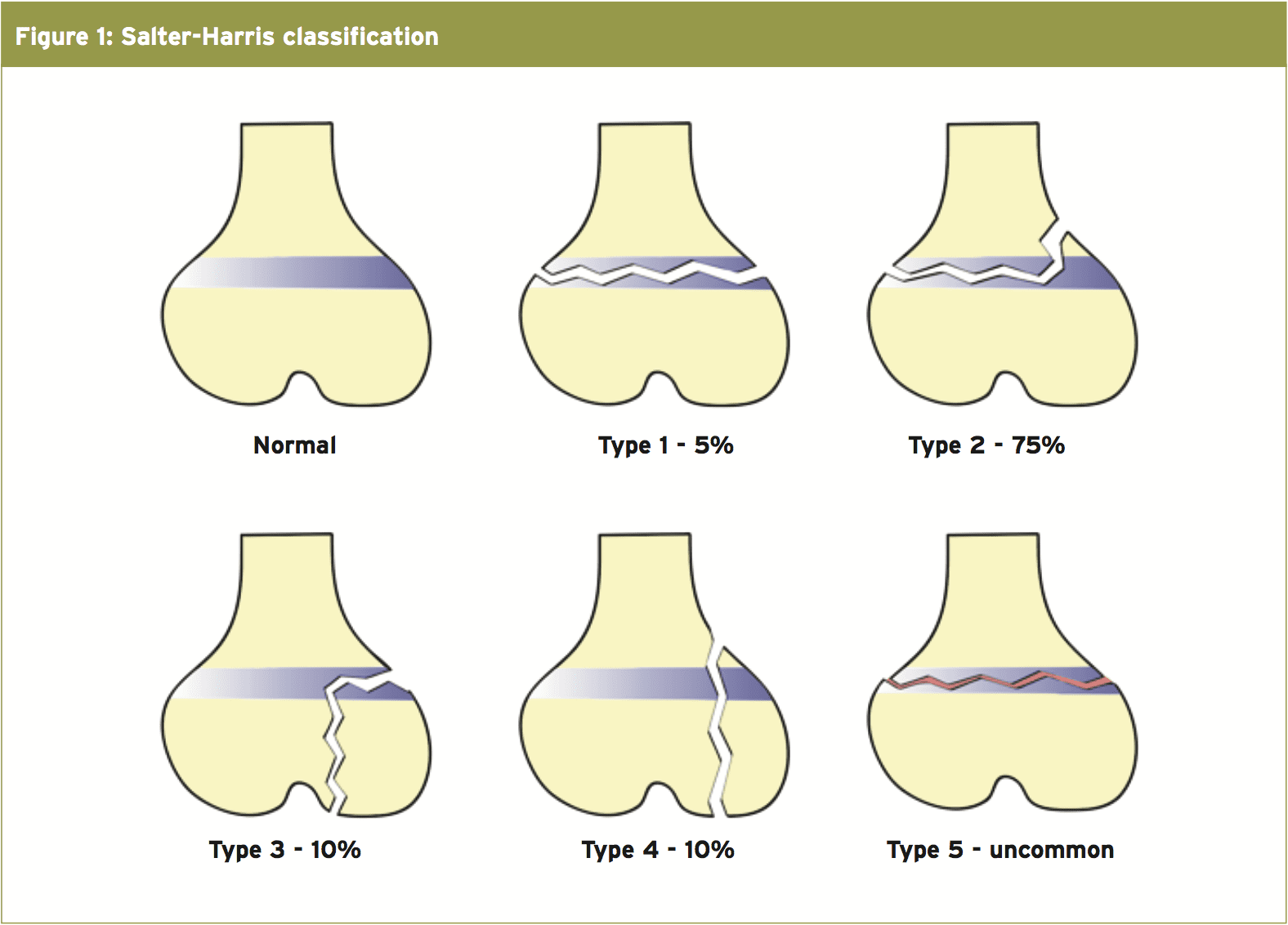
Epiphyseal fractures account for up to 30% of all childhood fractures, with 15% of these being affected by growth arrest in the form of angular deformity or leg length discrepancy(10). In order to manage them correctly, it is therefore important that we are suspicious of these injuries following a traumatic event. Epiphyseal fractures are diagnosed using the Salter-Harris classification as described in table 3 and figure 1.
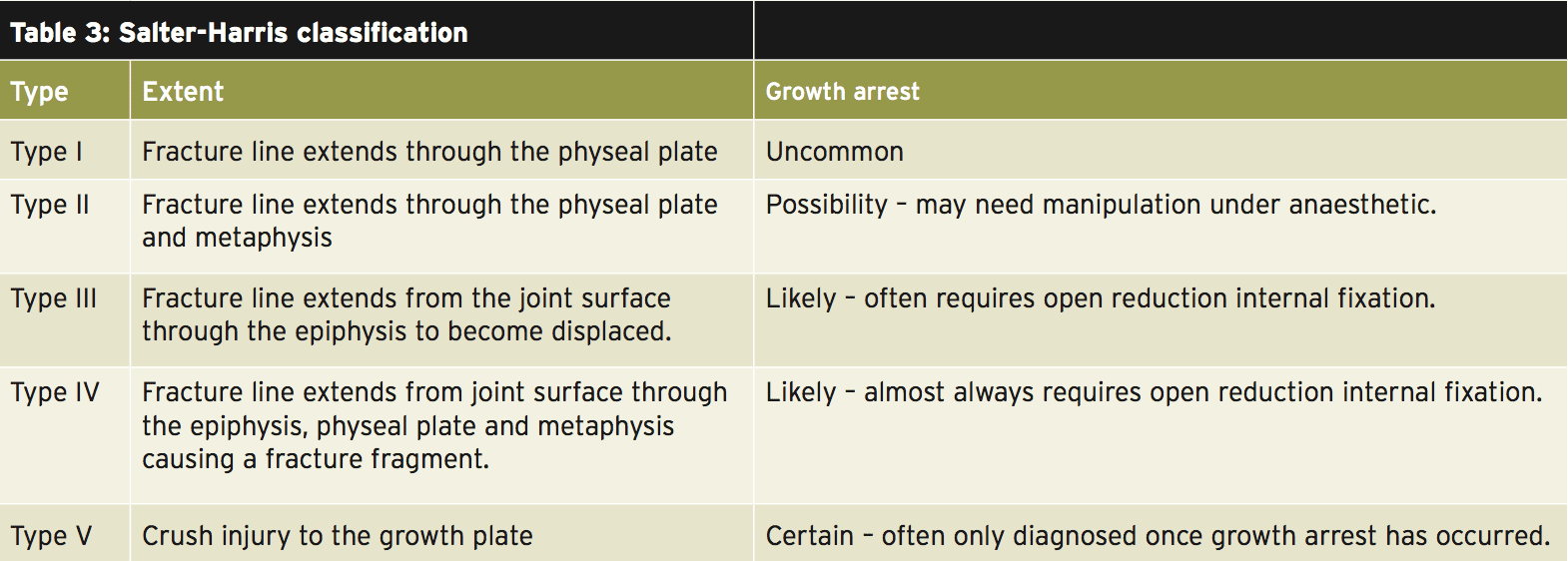
 Whether they are in a good or bad position, physeal injuries unite very quickly (due to the site-specific vascular supply and the already high levels of cellular activity); therefore early detection and reduction (if needed) is critical to reduce long-term growth defects.
Whether they are in a good or bad position, physeal injuries unite very quickly (due to the site-specific vascular supply and the already high levels of cellular activity); therefore early detection and reduction (if needed) is critical to reduce long-term growth defects.
All suspected injuries should be assessed by a doctor as soon as possible to reduce long-term problems. Type I Salter- Harris fractures account for 75% of this type of injury, and recovery is usually good with strengthening and a complete return to sport rehabilitation following 2-4 weeks of non-partial weight bearing. If any displacement has occurred, this is corrected with closed reduction, and the joint bone is manipulated into alignment without the need for surgery.
Type II injuries also need to undergo closed reduction if displacement is seen, followed by 4-6 weeks of no weight bearing, often while immobilized. Type III and IV injuries are less commonly seen but require open reduction and internal fixation followed by a period of reduced weight bearing and strict rehabilitation.
The uncommon, Type V or compression fracture injury is rarely identified prior to the occurrence of growth arrest, making it difficult for an athlete to return to his/her existing level of sport. Treatment focuses on correcting leg length discrepancy or deformity. All Salter-Harris fractures should be followed up by a doctor to monitor for any growth defects(4).
Prevention
By ensuring young athletes are strong enough to withstand forces and load placed on their joints epiphyseal and apophyseal injuries can be reduced. Bergarnon (2010) describes how excessive repeated loading, early specialization and insufficient recovery can lead to decreased positive adaptations in the musculoskeletal system, particularly in young athletes whose growth changes make them more vulnerable. Training should be periodized, with increased focus on flexibility, strength, prioprioception, technique and movement rather than heavy, repetitive loading and competition.
Strategies can easily be put in to place to minimise these and prevent athlete burnout. Athletes should be educated at an early age on the importance of recovery, and will likely benefit from this education being scheduled into their training programs.
Although many younger athletes transition from summer to winter sports, some kind of offseason, is important for athletes to recover, carry out rehab and prehabilitation, as well as expose themselves to other sports and experiences to aid their overall athletic development. Preseason should be structured so athletes are conditioned prior to competition and can reduce injury rates. Monitoring and screening is a crucial part of all athlete development. However, it should be carried out more regularly in young athletes in order to monitor growth spurts and times when they are at increased risk of joint surface injuries.
Much organized sport for young athletes does not adequately ensure suitable levels of strength, neuromuscular fitness, co-ordination and balance to meet the elite demands on the athletes. Therefore it is our responsibility as practitioners to educate athletes, coaches and parents about the differences between development phases, and considerations for training a younger population to minimize and appropriately manage injury. Ultimately, this will help ensure that athletes can reach their full sporting potential.
References
1. British Journal of Sports Medicine 2015, 49: 843-851
2. Clinical Journal of Sports Medicine 2014. 24: 3-20
3. Endocrinilogy and Metabolism 2015. 20(1):8-12
4. Sports Health 2009, 1(3): 201-211
5. Sport Journal 2014, 31; 304-326
6. Current Sports Medicine Reports 2010. 9(5):265-8
7. British Journal of Sports Medicine 2006. 40(9): 749-760
8. Current Sports Medicine Reports 2010 9(6):356-8
9. International Journal of Athletic Therapy and Training 2012. 17(2):5-9
10. International Journal of Sports Physical Therapy 2012. 7(6); 691-704
Post Disclaimer
Professional Scope of Practice *
The information herein on "Advice For Young Athletes" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Our information scope is limited to Chiropractic, musculoskeletal, physical medicines, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somatovisceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and/or functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.*
Our office has reasonably attempted to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez, DC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, RN*, CCST, IFMCP*, CIFM*, ATN*
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807, New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Florida
Florida License RN License # RN9617241 (Control No. 3558029)
License Compact Status: Multi-State License: Authorized to Practice in 40 States*
Presently Matriculated: ICHS: MSN* FNP (Family Nurse Practitioner Program)
Dr. Alex Jimenez DC, MSACP, RN* CIFM*, IFMCP*, ATN*, CCST
My Digital Business Card